- Record: found
- Abstract: found
- Article: found
Diagnostic Value and Prognostic Significance of Procalcitonin Combined with C-Reactive Protein in Patients with Bacterial Bloodstream Infection
Read this article at
Abstract
Objective
To study the clinical values and implications for the prognosis of procalcitonin (PCT) combined with C-reactive protein (hs-CRP) in patients with bacterial bloodstream infection.
Methods
One hundred and twenty patients with infection hospitalized from Mar. 2020 to Jun. 2021 were chosen as subjects. All participants were tested for serum PCT, hs-CRP, and blood culture. According to the types of pathogenic bacteria, they were divided into the gram-negative bacteria bloodstream infection group ( n = 53) and the gram-positive bacteria bloodstream infection group ( n = 31). Depending on the prognostic outcome of the participants after 28 days, they were categorized into survival and fatality cohorts. The PCT and hs-CRP levels were compared to explore diagnostic value implications for the prognosis of the cases with bacterial bloodstream infection.
Results
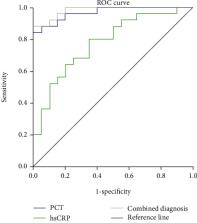
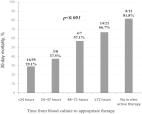
Serum PCT and hs-CRP values in the positive cohort were higher than those in the negative cohort. The levels of serum PCT and hs-CRP in pulmonary infection were higher than those in the group with negative cases, and the difference was statistically significant ( P < 0.05). There were 27 gram-positive participants and 9 gram-negative cases in the positive cohort. The serum PCT value of gram-negative bacterial infection was greater than that of gram-positive bacterial infection. The value of serum PCT in the gram-negative bacterial infection group was higher than that in the gram-positive bacterial infection group, and the difference was statistically significant ( P < 0.05). The areas under the curve (AUCs) of PCT, combination of hs-CRP and PCT, and hs-CRP were 0.946, 0.783, and 0.991, respectively. The combined examination of PCT and hs-CRP was the largest, PCT was the second, and hs-CRP was the lowest. These results indicated that the accuracy of combined detection of PCT and hs-CRP in the diagnostic bloodstream infection was the highest (0.991), followed by PCT (0.946) and the lowest (0.783). The PCT and hs-CRP levels of the survival cohort were lower than those in the death cohort. AUCs of PCT, hs-CRP and PCT, and hs-CRP were 0.848, 0.826, and 0.934, respectively. The combined examination of PCT and hs-CRP was the largest, followed by PCT and hs-CRP. The accuracy of the combination of PCT and hs-CRP was the highest (0.934), followed by PCT (0.848), and the diagnostic accuracy of hs-CRP was the lowest (0.826).
Conclusion
There were significant differences in the levels of PCT and CRP between the gram-positive bacteria group and the gram-positive bacteria group. PCT and CRP have high diagnostic values in predicting the short-term prognosis of patients. PCT and CRP assist clinical diagnosis and guide treatment and play a positive role in early treatment and prognosis evaluation of patients.
Related collections
Most cited references31

- Record: found
- Abstract: found
- Article: found
The Microbiology of Bloodstream Infection: 20-Year Trends from the SENTRY Antimicrobial Surveillance Program
- Record: found
- Abstract: found
- Article: not found
Burden of bacterial bloodstream infection—a brief update on epidemiology and significance of multidrug-resistant pathogens
- Record: found
- Abstract: found
- Article: found