- Record: found
- Abstract: found
- Article: found
Multimorbidity of communicable and non-communicable diseases in low- and middle-income countries: A systematic review
Read this article at
Abstract
Objective
The aim of this systematic review is to analyse existing evidence on prevalence, patterns, determinants, and healthcare challenges of communicable and non-communicable disease multimorbidity in low- and middle-income countries (LMICs).
Methods
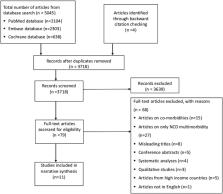
PubMed, Cochrane, and Embase databases were searched from 1 st January 2000 to 31 st July 2020. The National Institute of Health (NIH) quality assessment tool was used to critically appraise studies. Findings were summarized in a narrative synthesis. The review was registered with PROSPERO (CRD42019133453).
Results
Of 3718 articles screened, 79 articles underwent a full text review of which 11 were included for narrative synthesis. Studies reported on 4 to 20 chronic communicable and non-communicable diseases; prevalence of multimorbidity ranged from 13% in a study conducted among 242,952 participants from 48 LMICS to 87% in a study conducted among 491 participants in South Africa. Multimorbidity was positively associated with older age, female sex, unemployment, and physical inactivity. Significantly higher odds of multimorbidity were noted among obese participants (OR 2.33; 95% CI: 2.19–2.48) and those who consumed alcohol (OR 1.44; 95% CI: 1.25–1.66). The most frequently occurring dyads and triads were HIV and hypertension (23.3%) and HIV, hypertension, and diabetes (63%), respectively. Women and participants from low wealth quintiles reported higher utilization of public healthcare facilities.
Conclusion
The identification and prevention of risk factors and addressing evidence gaps in multimorbidity clustering is crucial to address the increasing communicable and non-communicable disease multimorbidity in LMICs. To identify communicable and non-communicable diseases trends over time and identify causal relationships, longitudinal studies are warranted.
Related collections
Most cited references47
- Record: found
- Abstract: not found
- Article: not found
Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.
- Record: found
- Abstract: found
- Article: not found
Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study.
- Record: found
- Abstract: found
- Article: not found