- Record: found
- Abstract: found
- Article: found
Non-communicable disease comorbidities in HIV patients: diabetes, hypertension, heart disease, and obstructive sleep apnea as a neglected issue
Read this article at
Abstract
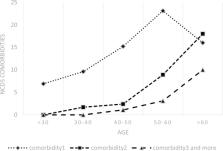
The present study evaluates the non-communicable disease (NCD) patterns and related risk factors among people living with HIV (PLWH) in Iran. This national cross-sectional survey study was conducted on 1173 confirmed PLWHs with a mean age of 35.35 (56.82 Over 50 years old, 33.90 Under 50 years old) admitted from 15 different provinces in the country. Logistic regression was used to analyze the association of factors with having at least one NCD comorbidity. From 1173 PLWH, 225(19.18%) participants experienced at least one NCD (15.20% and 38.69% among under- and over-50-year-old patients, respectively). The prevalence of heart disease, hypertension, diabetes, and sleep apnea among all patients was 1.59%, 2.05%, 1.55%, and 10.26%, respectively. The similar prevalence for each NCD among those over 50 years was 10.11%, 15.71%, 9.01%, 25.44%, and 1.01%, 1.12%, 1.04%, and 9.23% among those under 50 years, respectively. The odds of being at risk of at least one NCD stood higher in patients over 50 years (ORadj = 2.93, 95% CI 1.96–4.37), married (ORadj = 2.48, 95% CI 1.41–4.35), divorced or widowed (ORadj = 2.78, 95% CI 1.48–5.20), and obese (ORadj = 3.82, 95% CI 2.46–5.91). According to our findings regarding the prevalence of NCDs among patients under 50 years of age, we recommend that policymakers give greater consideration to this group in the screening and care programs for NCDs since adults and the elderly are both vulnerable to the risk factors for developing NCDs.
Related collections
Most cited references47
- Record: found
- Abstract: found
- Article: not found
Characteristics, Prevention, and Management of Cardiovascular Disease in People Living With HIV: A Scientific Statement From the American Heart Association
- Record: found
- Abstract: found
- Article: not found