- Record: found
- Abstract: found
- Article: found
Renal outcomes according to renal replacement therapy modality and treatment protocol in the ATN and RENAL trials
Read this article at
Abstract
Background
In critically ill patients with acute kidney injury, renal replacement therapy (RRT) modality and treatment protocols may affect kidney recovery. This study explored whether RRT modality and treatment protocol affected RRT dependence in the ‘Randomized Evaluation of Normal versus Augmented Level of RRT’ and the ‘Acute Renal Failure Trial Network’ (ATN) trials.
Methods
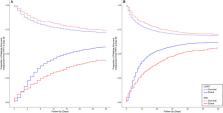
Primary outcome was 28-day RRT dependence. Secondary outcomes included RRT dependence among survivors and in different SOFA-based treatment protocol groups. We used the Fine-Gray competing-risk model sub-distribution hazard ratio (SHR) to assess the primary outcome. Analyses were adjusted for confounders.
Results
Of 2542 patients, 2175 (85.5%) received continuous RRT (CRRT) and 367 (14.4%) received intermittent hemodialysis (IHD) as first RRT modality. CRRT-first patients had greater illness severity. After adjustment, there was no between-group difference in 28-day RRT dependence (SHR, 0.96 [95% CI 0.84–1.10]; p = 0.570) or hospital mortality (odds ratio [OR], 1.14 [95% CI 0.86–1.52]; p = 0.361) However, among survivors, CRRT-first was associated with decreased 28-day RRT dependence (OR, 0.54 [95% CI 0.37–0.80]; p = 0.002) and more RRT-free days (common OR: 1.38 [95% CI 1.11–1.71]). Moreover, among CRRT-first patient, the ATN treatment protocol was associated with fewer RRT-free days, greater mortality, and a fourfold increase in RRT dependence at day 28.
Conclusions
There was no difference in RRT dependence at day 28 between IHD and CRRT. However, among survivors and after adjustment, both IHD-first and the ATN treatment protocol were strongly associated with greater risk of RRT dependence at 28 days after randomization.
Trial registration NCT00221013 registered September 22, 2005, and NCT00076219 registered January 19, 2004.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study.
- Record: found
- Abstract: not found
- Article: not found
Covariate balancing propensity score
- Record: found
- Abstract: found
- Article: not found