- Record: found
- Abstract: found
- Article: found
Comparison of remimazolam tosilate and propofol during induction and maintenance of general anesthesia in patients undergoing laparoscopic cholecystectomy: a prospective, single center, randomized controlled trial
Read this article at
Abstract
Background
Remimazolam tosilate (RT) is a new, ultrashort-acting benzodiazepine. Here, we investigated the efficacy and safety of RT for general anesthesia in patients undergoing Laparoscopic Cholecystectomy (LC).
Methods
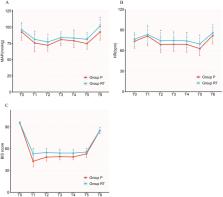
In this study, 122 patients undergoing laparoscopic cholecystectomy were randomly allocated to receive either remimazolam tosilate (Group RT) or propofol group (Group P). RT was administered as a slow bolus of 0.3 mg kg − 1 for induction, followed by 1.0–2.0 mg kg − 1 h − 1 for maintenance of general anesthesia. Propofol was started at 2 mg kg − 1 and followed by 4–10 mg kg − 1 h − 1 until the end of surgery. The primary outcome was the time to bispectral index (BIS) ≤ 60. The secondary outcome included the time to loss of consciousness (LoC), and the time to extubation. Adverse events were also assessed.
Results
A total of 112 patients were recruited for study participation. Among them, the time to BIS ≤ 60 in Group RT was longer than that in Group P (Group RT: 89.3 ± 10.7 s; Group P: 85.9 ± 9.7 s, P > 0.05). While the time to LoC comparing remimazolam and propofol showed no statistical significance (Group RT: 74.4 ± 10.3 s; Group P: 74.7 ± 9.3 s, P > 0.05). The time to extubation in Group RT was significantly longer than that in Group P (Group RT: 16.0 ± 2.6 min; Group P: 8.8 ± 4.3 min, P < 0.001). Remimazolam tosilate had more stable hemodynamics and a lower incidence of hypotension during general anesthesia.
Conclusions
Remimazolam tosilate can be safely and effectively used for general anesthesia in patients undergoing Laparoscopic Cholecystectomy. It maintains stable hemodynamics during induction and maintenance of general anesthesia compared with propofol. Further studies are needed to validate the findings.
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: not found
Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial.
- Record: found
- Abstract: found
- Article: not found
Efficacy and safety of remimazolam versus propofol for general anesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial
- Record: found
- Abstract: found
- Article: not found