- Record: found
- Abstract: found
- Article: found
A systematic review of symptomatic small bowel lipomas of the jejunum and ileum
Read this article at
Abstract
Introduction
Small bowel lipomas are rarely encountered benign adipose growths found within the small intestine wall or mesentery. Limited up-to-date evidence exists regarding such lipomas. We aim to aid clinical decision-making and improve patient outcomes through this comprehensive review.
Methodology
The terms ‘small bowel,’ ‘small intestine,’ ‘jejunum’ and ‘ileum’ were combined with ‘lipoma.’ EMBASE, Medline and PubMed database searches were performed. All papers published in English from 01/01/2000-31/12/2019 were included. Simple statistical analysis ( t-test, Anova) was performed.
Results
142 papers yielded 147 cases (adults = 138, pediatric = 9). Male = 88, female = 59 (average age = 49.9 years). Presenting symptoms: abdominal pain = 68.7%; nausea/vomiting = 35.3%, hematochezia/GI bleeding = 33.3%; anaemia = 10.9%; abdominal distension = 12.2%; constipation = 8.9%; weight loss = 7.5%. Mean preceding symptom length = 58.1 days (symptoms >1 year excluded (n = 9)). Diagnostic imaging utilised: abdominal X-Ray = 33.3%; endoscopy = 46.3%; CT = 78.2%; ultrasound = 23.8%. 124/137 (90.5%) required definitive surgical management (laparotomy = 89, laparoscopcic = 35). 9 patients were successfully managed endoscopically. Lipoma location: ileum = 59.9%, jejunum = 32%, mesentery = 4.8%. Maximal recorded lipoma size ranged 1.2–22 cm.
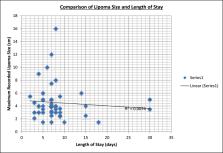
Mean maximum lipoma diameter and management strategy comparison: laparotomy 5.6 cm, laparoscopic = 4.4 cm, endoscopic = 3.7 cm, conservative = 4.5 cm. One-way Anova test, p value = 0.21. Average length of stay (LOS) was 7.4 days (range = 2–30). T-test p value = 0.13 when comparing management modalities and LOS. 4 complications, 0 mortality.
Conclusions
Important previously undocumented points are illustrated; a clearer symptom profile, diagnostic investigations utilised, size and site of lipomas, types and effectiveness of management modalities, associated morbidity and mortality. Open surgery remains the primary management. No statistically significant difference in LOS and lipoma size is demonstrated between management strategies. Endoscopic and laparoscopic techniques may reduce utilising invasive surgery in the future as skillset and availability improve.
Highlights
-
•
Up to date overview of symptomatic lipomas of the jejunum and ileum which no other paper has previously covered.
-
•
Highlights associated symptom profile, investigations, site and size of symptomatic lipomas, morbidity and mortality.
-
•
Evaluates the effectiveness of management strategies.
-
•
Offers a practical summary that may help guide other clinicians faced with similar presentations in the future.
Related collections
Most cited references35
- Record: found
- Abstract: found
- Article: not found
The diagnosis and management of adult intussusception.
- Record: found
- Abstract: found
- Article: not found
Colonoscopic perforation: incidence, risk factors, management and outcome.
- Record: found
- Abstract: found
- Article: not found