- Record: found
- Abstract: found
- Article: found
The severity and clinical characteristics of COVID-19 among patients with type 2 diabetes mellitus in Jazan, Saudi Arabia
Read this article at
Abstract
Background:
The objectives of the current study were to assess the severity and clinical characteristics of coronavirus disease 2019 (COVID-19) among Saudi adults with type 2 diabetes mellitus (T2DM) in Jazan region, Saudi Arabia.
Methods:
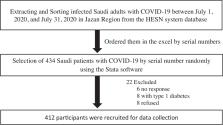
This retrospective cohort study included 412 patients with COVID-19 selected randomly from the Health Electronic Surveillance Network system, which contains the primary data on COVID-19 infections in Jazan.
Results:
COVID-19 disease duration was significantly longer in patients with T2DM (mean = 10.7 days) compared with those without T2DM (mean = 8.3 days) ( P = .01). Six (7%) patients experienced an increase in blood glucose concentrations and had to escalate their total daily insulin dose accordingly. Median fasting and random blood glucose levels increased after infection with COVID-19 (pre-COVID median = 119 and 172 mg/dL, respectively; post-COVID median = 148 and 216 mg/dL, respectively) ( P = .02). The total insulin dose pre-COVID (median = 42 units/d) increased after infection with COVID-19 (median = 58 units/d) ( P = .01). Most patients with T2DM had clinical COVID-19 symptoms (91%) and the remainder (9%) were asymptomatic. A large proportion (80%) of T2DM patients with mild COVID-19 symptoms self-isolated at home. COVID-19 patients with T2DM (11%) who had an oxygen saturation of ≤ 90% and admitted to the intensive care unit were higher than those without T2DM (5%) ( P = < .001). COVID-19 patients with T2DM (9%) had higher mortality rate than COVID-19 patients without T2DM (1%) ( P = < .001).
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study
- Record: found
- Abstract: found
- Article: found
Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area

- Record: found
- Abstract: found
- Article: found