- Record: found
- Abstract: found
- Article: found
Impact of perioperative blood transfusion on clinical outcomes in patients with colorectal liver metastasis after hepatectomy: a meta-analysis
Read this article at
Abstract
BACKGROUND
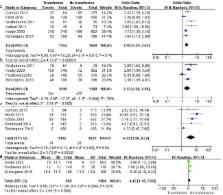
Perioperative blood transfusion may be associated with negative clinical outcomes in oncological surgery. A meta-analysis of published studies was conducted to evaluate the impact of blood transfusion on short- and long-term outcomes following liver resection of colorectal liver metastasis (CLM).
MATERIALS AND METHODS
A systematic search was performed to identify relevant articles. Data were pooled for meta-analysis using Review Manager version 5.3.
RESULTS
Twenty-five observational studies containing 10621 patients were subjected to the analysis. Compared with non-transfused patients, transfused patients experienced higher overall morbidity (odds ratio [OR], 1.98; 95% confidence intervals [CI] =1.49-2.33), more major complications (OR, 2.12; 95% CI =1.26-3.58), higher mortality (OR, 4.13; 95% CI =1.96-8.72), and longer length of hospital stay (weighted mean difference, 4.43; 95% CI =1.15-7.69). Transfusion was associated with reduced overall survival (risk ratio [RR], 1.24, 95% CI =1.11-1.38) and disease-free survival (RR, 1.38, 95% CI=1.23-1.56).
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
Inflammatory response, immunosuppression, and cancer recurrence after perioperative blood transfusions.
- Record: found
- Abstract: found
- Article: not found
Influence of transfusions on perioperative and long-term outcome in patients following hepatic resection for colorectal metastases.
- Record: found
- Abstract: found
- Article: not found