- Record: found
- Abstract: found
- Article: found
Safety of Redo Hepatectomy for Colorectal Liver Metastases after Selective Interarterial Radiation Therapy: A Case Report
Read this article at
Abstract
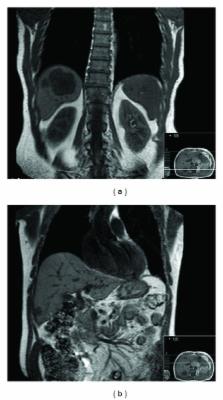
Surgical resection is the only potentially curative strategy in the treatment of patients with colorectal liver metastases (CLM). Unfortunately, only about 10%–15% of patients are candidates for resection. Preoperative chemotherapy aims to increase the number of patients that may be eligible for liver resection by downsizing liver metastases. For patients with unresectable, chemotherapy refractory CLM the available treatment options are limited. Selective interarterial radiation therapy (SIRT) is one of the most promising treatment options for this group of patients. Although only a small number of these patients have been reported as becoming candidates for potentially curative hepatic resection following sufficient reduction in the volume of liver metastases, the question arises regarding the safety of liver resection in these patients. We report a case of a patient who presented unresectable liver relapse of CLM after previous right hepatectomy. He underwent SIRT which resulted in downsizing of the liver metastases making the patient candidate for left lateral sectionectomy. He underwent the redo hepatectomy without any complications. To the best of our knowledge, this is the first reported case of redo hepatectomy after SIRT for CLM.
Related collections
Most cited references41
- Record: found
- Abstract: found
- Article: not found
Trends in long-term survival following liver resection for hepatic colorectal metastases.
- Record: found
- Abstract: found
- Article: not found
Hepatic radiation toxicity: avoidance and amelioration.
- Record: found
- Abstract: found
- Article: not found