- Record: found
- Abstract: found
- Article: found
Surgical options and reconstruction strategies for primary bone tumors of distal tibia: A systematic review of complications and functional outcome
Read this article at
Abstract
Background
Primary malignant or aggressive benign bone tumors rarely occur in distal tibia, and limb salvage remains the mainstay of surgical options. However, reconstruction methods for large bone defect after wide tumor resection in this location are debatable. The purpose of this systematical review is to critically evaluate each reconstruction method regarding the postoperative complications and functional outcome.
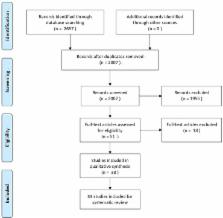
Methods
A systematic review of the 33 studies including 337 cases with tumors affecting distal tibia was performed after searching the PubMed and EMBASE databases. Pooled descriptive statistics with separate analyses for postoperative complications and functional outcome of different reconstruction options were performed.
Results
290 (86.1%) patients received limb salvage procedures. Reconstruction strategies including biological reconstruction, such as autograft, allograft, distraction osteogenesis and non-biological prosthetic replacement. The patients received limb salvage procedures tended to have a higher MSTS score (77.1% vs 70.9%, P = .055) and a higher incidence of local relapse (28/290 vs 0/47, P = .052) than those amputated. Biological reconstruction methods provided better functional outcome (78.4% vs 72.2%, P = .017) compared with non-biological prosthetic reconstruction, although similarity of incidence of major complications (51/253 vs 12/37, P = .091). With respect to the comparison between autograft and allograft reconstruction, the autograft seemed to have less major postoperative complications occurrence (27/165 vs 22/78, P = .032), and consequently better functional outcome (MSTS score, 80.2% vs 74.3%, P = .025) than allograft reconstruction.
Conclusions
Limb salvage results in better functional outcome compared with amputation. Biological reconstruction is more advocated than prosthetics replacement, and furthermore, autograft might be suggested to be the optimal reconstructive method with regard to better postoperative functional outcome and less major complications.
Related collections
Most cited references34
- Record: found
- Abstract: found
- Article: not found
Similar survival but better function for patients after limb salvage versus amputation for distal tibia osteosarcoma.
- Record: found
- Abstract: found
- Article: not found
Distal lower extremity sarcomas: frequency of occurrence and patient survival rate.
- Record: found
- Abstract: found
- Article: not found