- Record: found
- Abstract: found
- Article: not found
Clinical Characteristics and Differential Clinical Diagnosis of Novel Coronavirus Disease 2019 (COVID-19)
Read this article at
Abstract
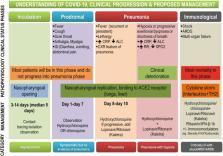
Novel Coronavirus Disease (COVID-19) has become a rapidly growing pandemic involving several nations. It is of serious concern and extreme challenge not only to the health personnel but also to the countries for containment. The causative organism is SARS-CoV-2, RNA virus of subgenus Sarbecovirus, similar to the SARS virus, and seventh member of the human coronavirus family responsible for this zoonotic infection. It binds to the human angiotensin converting enzyme (hACE-2) receptor and causes constitutional and respiratory symptoms. The major mode of transmission is human to human and the median incubation period is 4 days. The most common symptom as studied from various cohorts of COVID-19 patients are fever (83–98%) followed by fatigue (70%) and dry cough (59%); gastrointestinal symptoms are relatively uncommon differentiating it from SARS and MERS. Most of the SAR-CoV-2 infection are mild (80%) with a usual recovery period of 2 weeks. COVID-19 commonly affects males in the middle age and elderly age group, with highest case fatality (8–15%) among those aged >80 years. The disease begins with fever, dry cough, fatigue and myalgia progressing to dyspnoea and ARDS over 6 and 8 days post exposure, respectively. Underlying co-morbidities increase mortality in COVID-19. Poor prognostic factors are elderly, co-morbidities, severe lymphopaenia, high CRP and D-dimer >1 μg/L. The overall mortality rate ranges from 1.5 to 3.6%. COVID-19 has to be differentiated from other viral and bacterial pneumonias as they are more common among healthy adults. Despite constant and vigorous efforts by researchers and health agencies, we are far from containment, cure or prevention by vaccine; hence right information and stringent prevention and control measures are the only weapon in the armoury to combat the ongoing infection.
Related collections
Most cited references5
- Record: found
- Abstract: found
- Article: not found
Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study
- Record: found
- Abstract: found
- Article: not found
Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study
- Record: found
- Abstract: found
- Article: not found
