- Record: found
- Abstract: found
- Article: found
Efficacy of introducing a checklist to reduce central venous line associated bloodstream infections in the ICU caring for adult patients
Read this article at
Abstract
Background
Central line-associated bloodstream infections (CLABSI) are a major source of sepsis in modern intensive care medicine. Some years ago bundle interventions have been introduced to reduce CLABSI. The use of checklists may be an additional tool to improve the effect of these bundles even in highly specialized institutions. In this study we investigate if the introduction of a checklist reduces the frequency of CLABSI.
Methods
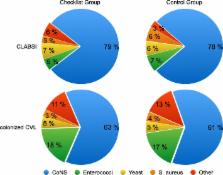
During the study period from October 2011 to September 2012, we investigated the effect of implementing a checklist for the placement of central venous lines (CVL). Patients were allocated either to the checklist group or to the control group, roughly in a 1:2 ratio. The frequency of CLABSI was compared between the two groups.
Results
During the study period 4416 CVL were inserted; 1518 in the checklist group and 2898 in the control group. The use of the checklist during CVL placement resulted in a lower CLABSI frequency. The incidence in the checklist group was 3.8 per 1000 catheter days as compared to 5.9 per 1000 catheter days in the control group (IRR = 0.57; p = 0.001). The use of the checklist also reduced the frequency of catheter colonisation significantly, 36.3 per 1000 catheter days in the checklist group vs 21.2 per 1000 catheter days in the control group, respectively (IRR = 0.58; p < 0.001).
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: found
Epidemiology of severe sepsis
- Record: found
- Abstract: found
- Article: not found
Optimal testing parameters for blood cultures.
- Record: found
- Abstract: found
- Article: not found