- Record: found
- Abstract: found
- Article: found
Incidence and outcome of salvage cystectomy after bladder sparing therapy for muscle invasive bladder cancer: a systematic review and meta-analysis
Read this article at
Abstract
Objective
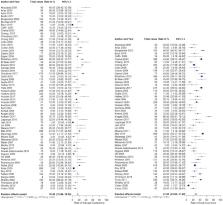
We conducted a systematic review and meta-analysis to assess the available literature regarding the surgical and oncologic outcomes of patients undergoing salvage radical cystectomy (SV-RC) for recurrence or failure of bladder sparing therapy (BST) for muscle-invasive bladder cancer (MIBC).
Methods
We searched MEDLINE (PubMed), EMBASE and Google Scholar databases in May 2020. We included all studies of patients with ≥ cT2N0/xM0 bladder cancer that were eligible for all treatment modalities at the time of treatment decision who underwent BST including radiotherapy (RTX). A meta-analysis was conducted to calculate the pooled rate of several variables associated with an increased need for SV-RC. Study quality and risk of bias were assessed using MINORS criteria.
Results
73 studies comprising 9110 patients were eligible for the meta-analysis. Weighted mean follow-up time was 61.1 months (range 12–144). The pooled rate of non-response to BST and local recurrence after BST, the two primary reasons for SV-RC, was 15.5% and 28.7%, respectively. The pooled rate of SV-RC was 19.2% for studies with a follow-up longer than 5 years. Only three studies provided a thorough report of complication rates after SV-RC. The overall complication rate ranged between 67 and 72% with a 30-day mortality rate of 0–8.8%. The pooled rates of 5 and 10-year disease-free survival after SV-RC were 54.3% and 45.6%, respectively.
Related collections
Most cited references115
- Record: found
- Abstract: found
- Article: not found
Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group.
- Record: found
- Abstract: found
- Article: not found
Methodological index for non-randomized studies (minors): development and validation of a new instrument.
- Record: found
- Abstract: found
- Article: not found