- Record: found
- Abstract: found
- Article: not found
Clinical and gonadal features and early surgical management of 45,X/46,XY and 45,X/47,XYY chromosomal mosaicism presenting with genital anomalies
Read this article at
Abstract
Objective
The 45,X/46,XY and 45,X/47,XYY group of patients includes some of those previously diagnosed with ‘mixed gonadal dysgenesis’. Our aim was to establish the clinical and gonadal spectrum, and early surgical management, of patients with chromosomal mosaicism presenting with genital anomalies.
Patients and methods
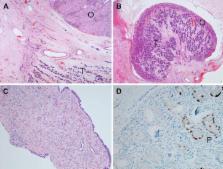
We performed a retrospective review of patients with 45,X/46,XY or 45,X/47,XYY mosaicism presenting with genital ambiguity between 1988 and 2009. At least one gonadal biopsy or gonadectomy specimen was available for each patient. Gonadal histology was re-evaluated by a paediatric pathologist.
Results
Of 31 patients with 45,X/46,XY ( n = 28) or 45,X/47,XYY ( n = 3) mosaicism and genital anomalies, 19 (61%) were raised male. Histology of 46 gonads was available from patients who had undergone a gonadectomy or gonadal biopsy, at a median age of 9.5 months. 18 gonads were palpable at presentation, including 5 (28%) histologically unremarkable testes, 2 streak gonads, and 1 dysgenetic gonad with distinct areas of testicular and ovarian stroma but no oocytes. All intra-abdominal gonads were found to be dysgenetic testes (of which 2 were noted to have pre-malignant changes) or streaks, apart from 1 histologically unremarkable testis. 15 (48%) patients had other anomalies, most commonly cardiac and renal; 4 (13%) had a Turner phenotype.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Germ cell tumors in the intersex gonad: old paths, new directions, moving frontiers.
- Record: found
- Abstract: found
- Article: not found
Holistic management of DSD
- Record: found
- Abstract: found
- Article: not found
