- Record: found
- Abstract: found
- Article: found
Association between the severity of constipation and sarcopenia in elderly adults: A single-center university hospital-based, cross-sectional study
Read this article at
Abstract
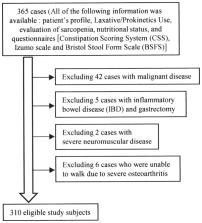
The aim of the present study was to investigate the association between the severity of constipation and sarcopenia in elderly adults. We conducted a single-center university hospital-based, retrospective cross-sectional study of consecutive outpatients aged ≥65 years from 2017 to 2020. Patients were included in the study if all of the following information were available from medical records: Patient's profile (age, sex, body mass index), laxative/prokinetics use, evaluation of sarcopenia, nutritional status, and questionnaires concerning the severity of constipation [Constipation Scoring System (CSS)], abdominal symptom-related quality of life (QOL) (Izumo scale) and stool shape [Bristol Stool Form Scale (BSFS)]. Multiple regression analysis of risk factors for high CSS score was performed. The results revealed that of the 310 eligible study subjects, [149 men (48.1%) and 161 women (51.9%); mean age, 75.7±6.1 years; mean body mass index, 23.0±3.6 kg/m 2], sarcopenia was noted in 83 cases (26.8%). The CSS score was significantly higher in the sarcopenia group than that noted in the non-sarcopenia group (4.9±4.9 vs. 3.6±3.6, P=0.009). The CSS score was significantly associated with the albumin level (r=-0.148), lymphocyte count (r=-0.118), CONUT score (r=0.130), reflux-related QOL score (r=0.155), upper abdominal pain-related QOL score (r=0.171), fullness-related QOL score (r=0.299), constipation-related QOL score (r=0.615), diarrhea-related QOL score (r=0.235) and BSFS score (r=-0.114). In multiple regression analysis, independent predictors for CSS score were sarcopenia [standardized partial regression coefficient (β)=0.107, P=0.032], constipation-related QOL score (β=0.537, P<0.001), laxative/prokinetics use (β=0.211, P<0.001) and BSFS score (β=-0.098, P=0.031) (R 2=0.436). In conclusion, sarcopenia, constipation-related QOL score, laxative/prokinetics use and BSFS score are associated with the severity of constipation in elderly adults.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment
- Record: found
- Abstract: found
- Article: not found
Stool form scale as a useful guide to intestinal transit time.
- Record: found
- Abstract: found
- Article: not found