- Record: found
- Abstract: found
- Article: found
Vitamin D deficiency is associated with sudden cardiac death, combined cardiovascular events, and mortality in haemodialysis patients
Read this article at
Abstract
Aims
Dialysis patients experience an excess mortality, predominantly of sudden cardiac death (SCD). Accumulating evidence suggests a role of vitamin D for myocardial and overall health. This study investigated the impact of vitamin D status on cardiovascular outcomes and fatal infections in haemodialysis patients.
Methods and results
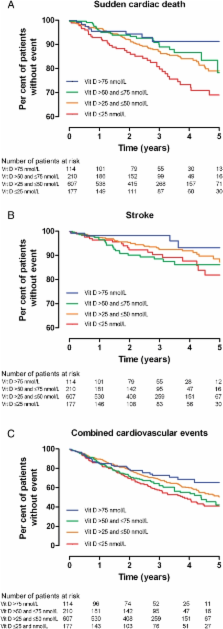
25-hydroxyvitamin D [25(OH)D] was measured in 1108 diabetic haemodialysis patients who participated in the German Diabetes and Dialysis Study and were followed up for a median of 4 years. By Cox regression analyses, we determined hazard ratios (HR) for pre-specified, adjudicated endpoints according to baseline 25(OH)D levels: SCD ( n = 146), myocardial infarction (MI, n = 174), stroke ( n = 89), cardiovascular events (CVE, n = 414), death due to heart failure ( n = 37), fatal infection ( n = 111), and all-cause mortality ( n = 545). Patients had a mean age of 66 ± 8 years (54% male) and median 25(OH)D of 39 nmol/L (interquartile range: 28–55). Patients with severe vitamin D deficiency [25(OH)D of≤ 25 nmol/L] had a 3-fold higher risk of SCD compared with those with sufficient 25(OH)D levels >75 nmol/L [HR: 2.99, 95% confidence interval (CI): 1.39–6.40]. Furthermore, CVE and all-cause mortality were strongly increased (HR: 1.78, 95% CI: 1.18–2.69, and HR: 1.74, 95% CI: 1.22–2.47, respectively), all persisting in multivariate models. There were borderline non-significant associations with stroke and fatal infection while MI and deaths due to heart failure were not meaningfully affected.
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis.
- Record: found
- Abstract: found
- Article: not found
25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study.
- Record: found
- Abstract: found
- Article: not found