- Record: found
- Abstract: found
- Article: found
Clinical Inertia in the Management of Type 2 Diabetes Mellitus: A Systematic Review
Read this article at
Abstract
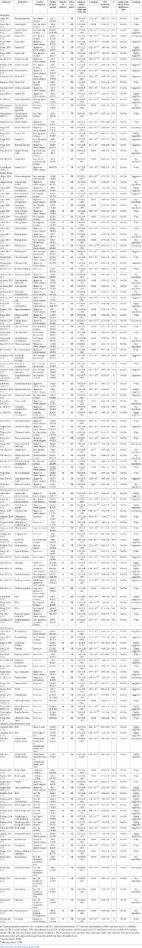
This review seeks to establish, through the recent available literature, the prevalence of therapeutic intensification delay and its sequences in poorly controlled Type 2 Diabetes Mellitus (T2DM) patients. The strategy identified studies exploring the clinical inertia and its associated factors in the treatment of patients with T2DM. A total of 25 studies meeting the pre-established quality criteria were included in this review. These studies were conducted between 2004 and 2021 and represented 575,067 patients diagnosed with T2DM. Trusted electronic bibliographic databases, including Medline, Embase, and the Cochrane Central Register of Controlled Trials, were used to collect studies by utilizing a comprehensive set of search terms to identify Medical Subject Headings (MeSH) terms. Most o the studies included in this review showed clinical inertia rates over 50% of T2DM patients. In the USA, clinical inertia ranged from 35.4% to 85.8%. In the UK, clinical inertia ranged from 22.1% to 69.1%. In Spain, clinical inertia ranged from 18.1% to 60%. In Canada, Brazil, and Thailand, clinical inertia was reported as 65.8%, 68%, and 68.4%, respectively. The highest clinical inertia was reported in the USA (85.8%). A significant number of patients with T2DM suffered from poor glycemic control for quite a long time before treatment intensification with oral antidiabetic drugs (OADs) or insulin. Barriers to treatment intensification exist at the provider, patient, and system levels. There are deficiencies pointed out by this review at specialized centers in terms of clinical inertia in the management of T2DM including in developed countries. This review shows that the earlier intensification in the T2DM treatment is appropriate to address issues around therapeutic inertia.
Related collections
Most cited references40

- Record: found
- Abstract: found
- Article: found
Risk factors for type 2 diabetes mellitus: An exposure-wide umbrella review of meta-analyses
- Record: found
- Abstract: found
- Article: not found