- Record: found
- Abstract: found
- Article: found
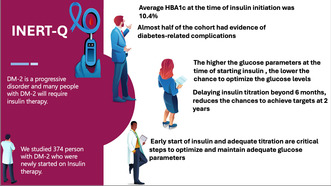
Insulin Inertia Among People With Type 2 Diabetes Mellitus in Qatar: The INERT‐Q Study

Read this article at
ABSTRACT
Background
Achieving and maintaining adequate glycaemic control is critical to reduce diabetes‐related complications. Therapeutic inertia is one of the leading causes of suboptimal glycaemic control.
Aim
To assess the degree of inertia in insulin initiation and intensification in people with Type 2 diabetes mellitus (DM‐2).
Methods
We performed a retrospective longitudinal cohort study and followed DM‐2 2 years before and 2 years after the start of insulin. The primary outcome was the proportion of patients who achieved glycaemic targets (HBA1c ≤ 7.5%) at 6th month, 1st year and 2nd year.
Results
We included 374 predominantly male subjects (62%). The mean age was 55.3 ± 11.3 years, the mean duration of DM‐2 was 12.0 ± 7.3 years, 64.4% were obese, 47.6% had a microvascular disease, and 24.3% had a macrovascular disease. The mean HBA1c at −2nd year and −1st year was 9.2 ± 2.1% and 9.3 ± 2.0%, respectively. The mean HbA1C at the time of insulin initiation was 10.4 ± 2.1%. The mean HBA1c at 6th month, 12th month and 2nd year was 8.5 ± 1.8%, 8.4 ± 1.8% and 8.5 ± 1.7%, respectively. The proportion of subjects who achieved HBA1c targets at 6th month, 12th month and 2nd year was 32.9%, 31.0% and 32.9%, respectively. Multivariate logistic regression analysis showed that achieving HBA1c targets at 6th month and 1st year increases the odds of achieving HBA1c targets at 2nd year (OR 4.87 [2.4–9.6] p < 0.001) and (OR 6.2 [3.2–12.0], p < 0.001), respectively.
Conclusion
In people with DM‐2, there was an alarming delay in starting and titrating insulin. The reduction in HBA1c plateaued at 6th month. Earlier initiation and intensification of insulin therapy are critical to achieving glycaemic targets. More studies are needed to examine the causes of therapeutic inertia from physicians', patients' and systems' points of view.
Abstract
-
Type 2 diabetes mellitus (DM‐2) is a progressive disease, and many patients require insulin therapy, particularly those with early‐onset disease.
-
Almost one‐third of the people with DM‐2 had evidence of complications at the time of insulin initiation.
-
The higher the HBA1c at the time of insulin initiation, the lower the chances of achieving glycaemic targets.
-
Delaying insulin titration beyond 6 months reduces the chances of achieving glycaemic targets at 2 years.
-
Earlier insulin initiation and adequate titration are critical to achieving glycaemic targets in people with poorly controlled DM‐2.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
A new equation to estimate glomerular filtration rate.
- Record: found
- Abstract: found
- Article: not found
IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045
- Record: found
- Abstract: found
- Article: not found