- Record: found
- Abstract: found
- Article: found
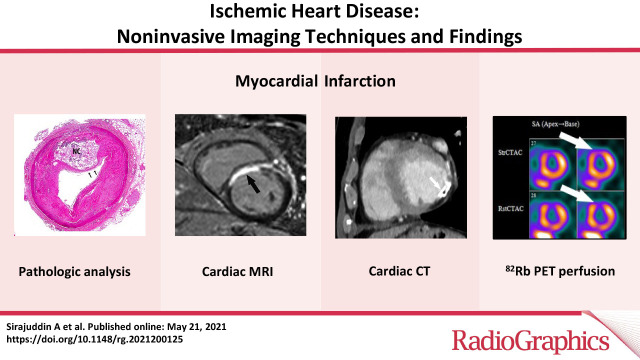
Ischemic Heart Disease: Noninvasive Imaging Techniques and Findings

Read this article at
Abstract
Ischemic heart disease is a leading cause of death worldwide and comprises a large proportion of annual health care expenditure. Management of ischemic heart disease is now best guided by the physiologic significance of coronary artery stenosis. Invasive coronary angiography is the standard for diagnosing coronary artery stenosis. However, it is expensive and has risks including vascular access site complications and contrast material–induced nephropathy. Invasive coronary angiography requires fractional flow reserve (FFR) measurement to determine the physiologic significance of a coronary artery stenosis. Multiple noninvasive cardiac imaging modalities can also anatomically delineate or functionally assess for significant coronary artery stenosis, as well as detect the presence of myocardial infarction (MI). While coronary CT angiography can help assess the degree of anatomic stenosis, its inability to assess the physiologic significance of lesions limits its specificity. Physiologic significance of coronary artery stenosis can be determined by cardiac MR vasodilator or dobutamine stress imaging, CT stress perfusion imaging, FFR CT, PET myocardial perfusion imaging (MPI), SPECT MPI, and stress echocardiography. Clinically unrecognized MI, another clear indicator of physiologically significant coronary artery disease, is relatively common and is best evaluated with cardiac MRI. The authors illustrate the spectrum of imaging findings of ischemic heart disease (coronary artery disease, myocardial ischemia, and MI); highlight the advantages and disadvantages of the various noninvasive imaging methods used to assess ischemic heart disease, as illustrated by recent clinical trials; and summarize current indications and contraindications for noninvasive imaging techniques for detection of ischemic heart disease.
Online supplemental material is available for this article.
Published under a CC BY 4.0 license.
Abstract
Related collections
Most cited references116
- Record: found
- Abstract: found
- Article: not found
Heart Disease and Stroke Statistics—2020 Update
- Record: found
- Abstract: found
- Article: not found
Mechanisms of plaque formation and rupture.
- Record: found
- Abstract: found
- Article: not found