Contributors
Jenna H. Sobey:
ORCID: http://orcid.org/0000-0003-4480-146X
Role: ConceptualizationRole: Data curationRole: Formal analysisRole: InvestigationRole:
MethodologyRole: ValidationRole: Writing – original draftRole: Writing – review &
editing
Srijaya K. Reddy:
ORCID: http://orcid.org/0000-0002-1924-8976
Role: InvestigationRole: ValidationRole: Writing – original draftRole: Writing – review
& editing
Kyle M. Hocking:
ORCID: http://orcid.org/0000-0002-3603-7185
Role: ConceptualizationRole: Data curationRole: Formal analysisRole: InvestigationRole:
MethodologyRole: ResourcesRole: SoftwareRole: ValidationRole: Writing – original draftRole:
Writing – review & editing
Monica E. Polcz: Role: ConceptualizationRole: Data curationRole: Formal analysisRole: InvestigationRole:
ValidationRole: Writing – original draftRole: Writing – review & editing
Christy M. Guth: Role: ConceptualizationRole: Data curationRole: Formal analysisRole: InvestigationRole:
ValidationRole: Writing – original draftRole: Writing – review & editing
Cameron Schlegel: Role: ConceptualizationRole: Data curationRole: Formal analysisRole: InvestigationRole:
ValidationRole: Writing – original draftRole: Writing – review & editing
Jon Whitfield: Role: ConceptualizationRole: Data curationRole: Formal analysisRole: InvestigationRole:
MethodologyRole: ResourcesRole: SoftwareRole: Writing – review & editing
Susan S. Eagle: Role: ConceptualizationRole: Data curationRole: InvestigationRole: MethodologyRole:
Writing – review & editing
Colleen M. Brophy: Role: ConceptualizationRole: Data curationRole: Formal analysisRole: InvestigationRole:
MethodologyRole: ResourcesRole: SupervisionRole: Writing – review & editing
Bret D. Alvis: Role: ConceptualizationRole: Data curationRole: Formal analysisRole: InvestigationRole:
MethodologyRole: SupervisionRole: ValidationRole: Writing – original draftRole: Writing
– review & editing
Georg M. Schmölzer: Role: Editor
Journal
Journal ID (nlm-ta): PLoS One
Journal ID (iso-abbrev): PLoS ONE
Journal ID (publisher-id): plos
Journal ID (pmc): plosone
Title:
PLoS ONE
Publisher:
Public Library of Science
(San Francisco, CA USA
)
ISSN
(Electronic):
1932-6203
Publication date
(Electronic):
8
July
2020
Publication date Collection: 2020
Volume: 15
Issue: 7
Electronic Location Identifier: e0235933
Affiliations
[1
]
Department of Anesthesiology, Division of Pediatric Anesthesiology, Monroe Carell
Jr. Children’s Hospital at Vanderbilt University Medical Center / Vanderbilt University
School of Medicine, Nashville, Tennessee, United States of America
[2
]
Department of Surgery, Vanderbilt University Medical Center / Vanderbilt University
School of Medicine, Nashville, Tennessee, United States of America
[3
]
VoluMetrix, LLC, Nashville, TN, United States of America
[4
]
Department of Anesthesiology, Division of Cardiothoracic Anesthesiology, Vanderbilt
University Medical Center / Vanderbilt University School of Medicine, Nashville, Tennessee,
United States of America
[5
]
Department of Surgery, Division of Vascular Surgery, Vanderbilt University Medical
Center / Vanderbilt University School of Medicine, Nashville, Tennessee, United States
of America
[6
]
Department of Anesthesiology, Division of Critical Care Medicine, Vanderbilt University
Medical Center / Vanderbilt University School of Medicine, Nashville, Tennessee, United
States of America
University of Alberta, CANADA
Author notes
Competing Interests: The intellectual property associated with this novel technology is held by Vanderbilt
University Medical Center (VUMC) and licensed to VoluMetrix. VoluMetrix was not a
funding source for this study. KMH is Founder, CEO and President of VoluMetrix and
an inventor on intellectual property in the field of venous waveform analysis assigned
to VUMC and licensed to VoluMetrix. CMB is Founder and CMO of VoluMetrix and an inventor
on intellectual property in the field of venous waveform analysis assigned to VUMC
and licensed to VoluMetrix. BDA, is CSO and owns stock in VoluMetrix and is an inventor
on intellectual property in the field of venous waveform analysis assigned to VUMC
and licensed to VoluMetrix and is married to the COO of VoluMetrix. JW is the Senior
Software Engineer and owns stock in VoluMetrix. SSE was former CEO of VoluMetrix and
an inventor on intellectual property in the field of venous waveform analysis assigned
to VUMC and licensed to VoluMetrix. The remaining authors have no conflicts of interest
to declare. These declarations do not alter our adherence to PLOS ONE policies on
sharing data and materials.
Author information
Article
Publisher ID:
PONE-D-20-15303
DOI: 10.1371/journal.pone.0235933
PMC ID: 7343152
PubMed ID: 32640004
SO-VID: 2ba4b37a-511a-4c3b-8a93-1b58af45a46d
Copyright © © 2020 Sobey et al
License:
This is an open access article distributed under the terms of the
Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided
the original author and source are credited.
History
Date
received
: 21
May
2020
Date
accepted
: 24
June
2020
Page count
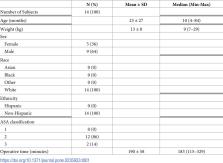
Figures: 1,
Tables: 1,
Pages: 8
Funding
Funded by: funder-id http://dx.doi.org/10.13039/501100008982, National Science Foundation;
Award ID: 1549576
Award Recipient
:
ORCID: http://orcid.org/0000-0002-3603-7185
Kyle M. Hocking
This research work was supported by the National Science Foundation (NSF), grant number
1549576 (PI: KMH). VoluMetrix WAS NOT a funding organization. The funder (NSF) provided
support in the form of salary support (KMH, BA, SE), and prototype development, but
did not have a role in the study design, data collection and analysis, decision to
publish, or preparation of the manuscript. The specific roles of these authors are
articulated in the ‘author contributions’ sections.
Categories
Subject:
Research Article
Subject:
Medicine and Health Sciences
Subject:
Pediatrics
Subject:
Medicine and Health Sciences
Subject:
Surgical and Invasive Medical Procedures
Subject:
Pediatric Surgery
Subject:
Medicine and Health Sciences
Subject:
Surgical and Invasive Medical Procedures
Subject:
Medicine and Health Sciences
Subject:
Vascular Medicine
Subject:
Blood Pressure
Subject:
Medicine and Health Sciences
Subject:
Hematology
Subject:
Hemodynamics
Subject:
Biology and Life Sciences
Subject:
Anatomy
Subject:
Musculoskeletal System
Subject:
Body Limbs
Subject:
Arms
Subject:
Wrist
Subject:
Medicine and Health Sciences
Subject:
Anatomy
Subject:
Musculoskeletal System
Subject:
Body Limbs
Subject:
Arms
Subject:
Wrist
Subject:
Medicine and Health Sciences
Subject:
Critical Care and Emergency Medicine
Subject:
Resuscitation
Subject:
Biology and Life Sciences
Subject:
Anatomy
Subject:
Body Fluids
Subject:
Blood
Subject:
Blood Volume
Subject:
Medicine and Health Sciences
Subject:
Anatomy
Subject:
Body Fluids
Subject:
Blood
Subject:
Blood Volume
Subject:
Biology and Life Sciences
Subject:
Physiology
Subject:
Body Fluids
Subject:
Blood
Subject:
Blood Volume
Subject:
Medicine and Health Sciences
Subject:
Physiology
Subject:
Body Fluids
Subject:
Blood
Subject:
Blood Volume
Custom metadata