- Record: found
- Abstract: found
- Article: found
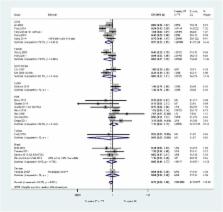
CYP genetic variants and toxicity related to anti-tubercular agents: a systematic review and meta-analysis
Read this article at
Abstract
Background
Treatment with anti-tuberculosis drugs may cause patients to experience serious adverse effects. Genetic factors, such as polymorphisms of CYP genes, may increase the likelihood of a patient experiencing such adverse drug reactions. In this systematic review and meta-analysis, we synthesised evidence for associations between CYP genetic variants and anti-tuberculosis drug-related toxicity outcomes.
Methods
We searched MEDLINE, PubMed, EMBASE, BIOSIS and Web of Science to identify relevant studies. We performed meta-analyses to obtain an effect estimate for each genetic variant on each outcome, and stratified all analyses by country. We qualitatively assessed the methodological quality of the included studies.
Results
We included data from 28 distinct cohorts of patients in the review. We identified many areas of concern with regard to the quality of included studies. Patients with homozygous mutant-type or heterozygous genotype at the CYP2E1 RsaI polymorphism were significantly less likely to experience hepatotoxicity than patients with homozygous wild-type genotype (odds ratio [OR] = 0.75, 95% confidence interval [CI] 0.56–1.00; p = 0.047, I 2 = 58.2%). No significant differences were observed for the CYP2E1 DraI and PstI polymorphisms. For the 96-bp deletion-insertion single-nucleotide polymorphism (SNP) of the CYP2E1 gene, homozygous mutant-type significantly increased hepatotoxicity risk compared with homozygous wild-type (OR = 8.20, 95% CI 1.38–48.68, I 2 = 0%); no significant difference was observed for heterozygous genotype compared with homozygous wild-type (OR = 0.77, 95% CI 0.19–3.21, I 2 = 0%).
Conclusions
Generally, we identified that coverage of the association between SNPs of CYP genes and anti-tuberculosis drug-related toxicity outcomes is incomplete. We observed significant associations between the RsaI and 96-bp deletion-insertion SNPs of the CYP2E1 gene and anti-tuberculosis drug-related hepatotoxicity. We were unable to comment on the impact of ethnicity on the investigated associations, as information on participants’ ethnicity was sparsely reported in the included studies.
Related collections
Most cited references50

- Record: found
- Abstract: found
- Article: found
Worldwide Distribution of Cytochrome P450 Alleles: A Meta‐analysis of Population‐scale Sequencing Projects
- Record: found
- Abstract: found
- Article: not found
Cytochrome P450 2E1 genotype and the susceptibility to antituberculosis drug-induced hepatitis.
- Record: found
- Abstract: found
- Article: not found