- Record: found
- Abstract: found
- Article: found
The Therapeuatic Effect of Endostar on Soft Carotid Plaque Neovascularization in Patients with Non-small Cell Lung Cancer
Read this article at
Abstract
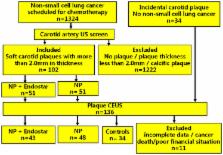
The purpose of this study was to investigate the effect of the angiogenesis inhibitor Endostar on carotid plaque neovascularization in patients with non-small cell lung cancer (NSCLC) using contrast-enhanced ultrasound (CEUS). Ninety-one patients who had NSCLC with soft carotid plaques were selected for treatment either with the NP regimen (vinorelbine + cisplatin) (43 patients) or with the ENP regimen (Endostar + NP) (48 patients). Plaque thickness and neovascularization of the plaque were assessed before and at 1 month after treatment using CEUS. Enhanced intensity (EI) of CEUS was used for quantification of plaque neovascularization. There was no significant changes in any group in thickness of plaque between recruitment and 1 month after treatment ( P > 0.05 for all). There was no significant change in the EI of plaque in the controls or NP groups at 1 month after treatment ( P > 0.05), while EI in the ENP group was significantly reduced at 1 month after treatment ( P < 0.01) and significantly lower than that in the controls or NP group at 1 month after treatment ( P < 0.001 both). This study indicates that carotid soft plaque neovascularization in patients with NSCLC can be reduced by anti-angiogenesis treatment.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
Plaque neovascularization is increased in ruptured atherosclerotic lesions of human aorta: implications for plaque vulnerability.
- Record: found
- Abstract: found
- Article: not found
Angiogenesis inhibitors endostatin or TNP-470 reduce intimal neovascularization and plaque growth in apolipoprotein E-deficient mice.
- Record: found
- Abstract: found
- Article: not found