- Record: found
- Abstract: found
- Article: found
Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways
Read this article at
Abstract
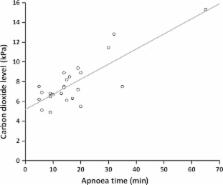
Emergency and difficult tracheal intubations are hazardous undertakings where successive laryngoscopy–hypoxaemia–re-oxygenation cycles can escalate to airway loss and the ‘can't intubate, can't ventilate’ scenario. Between 2013 and 2014, we extended the apnoea times of 25 patients with difficult airways who were undergoing general anaesthesia for hypopharyngeal or laryngotracheal surgery. This was achieved through continuous delivery of transnasal high-flow humidified oxygen, initially to provide pre-oxygenation, and continuing as post-oxygenation during intravenous induction of anaesthesia and neuromuscular blockade until a definitive airway was secured. Apnoea time commenced at administration of neuromuscular blockade and ended with commencement of jet ventilation, positive-pressure ventilation or recommencement of spontaneous ventilation. During this time, upper airway patency was maintained with jaw-thrust. Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE) was used in 15 males and 10 females. Mean (SD [range]) age at treatment was 49 (15 [25–81]) years. The median (IQR [range]) Mallampati grade was 3 (2–3 [2–4]) and direct laryngoscopy grade was 3 (3–3 [2–4]). There were 12 obese patients and nine patients were stridulous. The median (IQR [range]) apnoea time was 14 (9–19 [5–65]) min. No patient experienced arterial desaturation < 90%. Mean (SD [range]) post-apnoea end-tidal (and in four patients, arterial) carbon dioxide level was 7.8 (2.4 [4.9–15.3]) kPa. The rate of increase in end-tidal carbon dioxide was 0.15 kPa.min −1. We conclude that THRIVE combines the benefits of ‘classical’ apnoeic oxygenation with continuous positive airway pressure and gaseous exchange through flow-dependent deadspace flushing. It has the potential to transform the practice of anaesthesia by changing the nature of securing a definitive airway in emergency and difficult intubations from a pressured stop–start process to a smooth and unhurried undertaking.
Related collections
Most cited references42
- Record: found
- Abstract: found
- Article: not found
High-flow oxygen therapy in acute respiratory failure.
- Record: found
- Abstract: found
- Article: found