- Record: found
- Abstract: found
- Article: found
Pulmonary fat embolism and related effects during femoral intramedullary surgery: An experimental study in dogs

Read this article at
Abstract
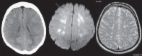
The aim of the present study was to develop an animal model of pulmonary fat embolism (PFE) caused by femoral intramedullary procedures, and to investigate the initial changes in the hemodynamics, cytokines and risk factors of PFE. Sixteen dogs were randomly divided into two groups: Group A (intramedullary reaming and bone cement injection, n=8) and Group B (surgical approach without opening the medullary cavity, n=8). The hemodynamics, arterial blood gases and relevant cytokines were evaluated, and the lungs were examined using Oil Red O staining. In the animals of Group A, the heart rate, central venous pressure, mean pulmonary arterial pressure, pulmonary capillary wedge pressure and extravascular lung water (EVLW) were increased compared with the baseline levels, while the mean arterial pressure was decreased immediately following the reaming and bone cement infusion (P<0.05). Furthermore, there was a significant reduction in the pH and the arterial oxygen tension (PaO 2), and a significant increase in the arterial carbon dioxide tension (PaCO 2; P<0.05 for all) following the bilateral intramedullary surgery. The EVLW was correlated with the PaO 2 (P<0.001) and PaCO 2 (P=0.046). Following surgery, there was a significant increase in tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β) and IL-6 levels in Group A (P<0.05). However, there were no significant changes in these parameters in Group B. The parameters tested, with the exception of pH, were significantly different in Group A compared with those in Group B (P<0.05) following the bilateral intramedullary surgery. Oil Red O staining was positive for all animals in Group A and negative for those in Group B. Femoral intramedullary surgery may induce PFE and subsequently affect hemodynamics and arterial blood gases. EVLW was correlated with the PaO 2 (P<0.001) and the PaCO 2 (P=0.046). These results demonstrated that EVLW and cytokines may serve as predictors of the development of fat embolism syndrome (FES).
Related collections
Most cited references29
- Record: found
- Abstract: found
- Article: found
Emergency management of fat embolism syndrome
- Record: found
- Abstract: found
- Article: not found
Accurate characterization of extravascular lung water in acute respiratory distress syndrome.
- Record: found
- Abstract: found
- Article: not found