- Record: found
- Abstract: found
- Article: found
Nuclear imaging of liposomal drug delivery systems: A critical review of radiolabelling methods and applications in nanomedicine
Read this article at
Abstract
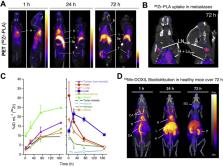
The integration of nuclear imaging with nanomedicine is a powerful tool for efficient development and clinical translation of liposomal drug delivery systems. Furthermore, it may allow highly efficient imaging-guided personalised treatments. In this article, we critically review methods available for radiolabelling liposomes. We discuss the influence that the radiolabelling methods can have on their biodistribution and highlight the often-overlooked possibility of misinterpretation of results due to decomposition in vivo. We stress the need for knowing the biodistribution/pharmacokinetics of both the radiolabelled liposomal components and free radionuclides in order to confidently evaluate the images, as they often share excretion pathways with intact liposomes ( e.g. phospholipids, metallic radionuclides) and even show significant tumour uptake by themselves ( e.g. some radionuclides). Finally, we describe preclinical and clinical studies using radiolabelled liposomes and discuss their impact in supporting liposomal drug development and clinical translation in several diseases, including personalised nanomedicine approaches.
Graphical abstract
Related collections
Most cited references288
- Record: found
- Abstract: found
- Article: not found
Tumor targeting via EPR: Strategies to enhance patient responses
- Record: found
- Abstract: found
- Article: not found
A molecular imaging primer: modalities, imaging agents, and applications.
- Record: found
- Abstract: not found
- Article: not found
