- Record: found
- Abstract: found
- Article: found
Angiotensin converting enzyme inhibitors and risk of lung cancer: population based cohort study
Read this article at
Abstract
Objective
To determine whether the use of angiotensin converting enzyme inhibitors (ACEIs), compared with use of angiotensin receptor blockers, is associated with an increased risk of lung cancer.
Participants
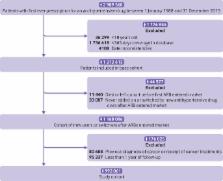
A cohort of 992 061 patients newly treated with antihypertensive drugs between 1 January 1995 and 31 December 2015 was identified and followed until 31 December 2016.
Main outcome measures
Cox proportional hazards models were used to estimate adjusted hazard ratios with 95% confidence intervals of incident lung cancer associated with the time varying use of ACEIs, compared with use of angiotensin receptor blockers, overall, by cumulative duration of use, and by time since initiation.
Results
The cohort was followed for a mean of 6.4 (SD 4.7) years, generating 7952 incident lung cancer events (crude incidence 1.3 (95% confidence interval 1.2 to 1.3) per 1000 person years). Overall, use of ACEIs was associated with an increased risk of lung cancer (incidence rate 1.6 v 1.2 per 1000 person years; hazard ratio 1.14, 95% confidence interval 1.01 to 1.29), compared with use of angiotensin receptor blockers. Hazard ratios gradually increased with longer durations of use, with an association evident after five years of use (hazard ratio 1.22, 1.06 to 1.40) and peaking after more than 10 years of use (1.31, 1.08 to 1.59). Similar findings were observed with time since initiation.
Conclusions
In this population based cohort study, the use of ACEIs was associated with an increased risk of lung cancer. The association was particularly elevated among people using ACEIs for more than five years. Additional studies, with long term follow-up, are needed to investigate the effects of these drugs on incidence of lung cancer.
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men.
- Record: found
- Abstract: found
- Article: not found