- Record: found
- Abstract: found
- Article: found
Video capsule endoscopy vs double-balloon enteroscopy in the diagnosis of small bowel bleeding: A systematic review and meta-analysis
Read this article at
Abstract
AIM
To compare the diagnostic accuracy of video capsule endoscopy (VCE) and double-balloon enteroscopy (DBE) in cases of obscure gastrointestinal bleeding (OGIB) of vascular origin.
METHODS
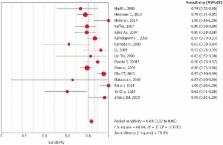
MEDLINE ( via PubMed), LILACS ( via BVS) and Cochrane/CENTRAL virtual databases were searched for studies dated before 2017. We identified prospective and retrospective studies, including observational, cohort, single-blinded and multicenter studies, comparing VCE and DBE for the diagnosis of OGIB, and data of all the vascular sources of bleeding were collected. All patients were subjected to the same gold standard method. Relevant data were then extracted from each included study using a standardized extraction form. We calculated study variables (sensitivity, specificity, prevalence, positive and negative predictive values and accuracy) and performed a meta-analysis using Meta-Disc software.
RESULTS
In the per-patient analysis, 17 studies (1477 lesions) were included. We identified 3150 exams (1722 VCE and 1428 DBE) in 2043 patients and identified 2248 sources of bleeding, 1467 of which were from vascular lesions. Of these lesions, 864 (58.5%) were diagnosed by VCE, and 613 (41.5%) were diagnosed by DBE. The pretest probability for bleeding of vascular origin was 54.34%. The sensitivity of DBE was 84% (95%CI: 0.82-0.86; heterogeneity: 78.00%), and the specificity was 92% (95%CI: 0.89-0.94; heterogeneity: 92.0%). For DBE, the positive likelihood ratio was 11.29 (95%CI: 4.83-26.40; heterogeneity: 91.6%), and the negative likelihood ratio was 0.20 (95%CI: 0.15-0.27; heterogeneity: 67.3%). Performing DBE after CE increased the diagnostic yield of vascular lesion by 7%, from 83% to 90%.
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
Wireless capsule endoscopy.
- Record: found
- Abstract: found
- Article: not found
Diagnostic value of endoscopic capsule in patients with obscure digestive bleeding: blinded comparison with video push-enteroscopy.
- Record: found
- Abstract: found
- Article: not found