- Record: found
- Abstract: found
- Article: found
Describing financial toxicity among cancer patients in different income countries: a systematic review and meta-analysis
Read this article at
Abstract
Background
There is limited evidence of financial toxicity (FT) among cancer patients from countries of various income levels. Hence, this study aimed to determine the prevalence of objective and subjective FT and their measurements in relation to cancer treatment.
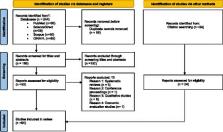
Methods
PubMed, Science Direct, Scopus, and CINAHL databases were searched to find studies that examined FT. There was no limit on the design or setting of the study. Random-effects meta-analysis was utilized to obtain the pooled prevalence of objective FT.
Results
Out of 244 identified studies during the initial screening, only 64 studies were included in this review. The catastrophic health expenditure (CHE) method was often used in the included studies to determine the objective FT. The pooled prevalence of CHE was 47% (95% CI: 24.0–70.0) in middle- and high-income countries, and the highest percentage was noted in low-income countries (74.4%). A total of 30 studies focused on subjective FT, of which 9 used the Comprehensive Score for FT (COST) tool and reported median scores ranging between 17.0 and 31.9.
Related collections
Most cited references91
- Record: found
- Abstract: found
- Article: not found
Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries

- Record: found
- Abstract: found
- Article: found