- Record: found
- Abstract: found
- Article: not found
The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients
Read this article at
Abstract
Objective
To estimate the mortality and length of stay in the intensive care unit (ICU) attributable to clinically important gastrointestinal bleeding in mechanically ventilated critically ill patients.
Design
Three strategies were used to estimate the mortality attributable to bleeding in two multicentre databases. The first method matched patients who bled with those who did not (matched cohort), using duration of ICU stay prior to the bleed, each of six domains of the Multiple Organ Dysfunction Score (MODS) measured 3 days prior to the bleed, APACHE II score, age, admitting diagnosis, and duration of mechanical ventilation. The second approach employed Cox proportional hazards regression to match bleeding and non-bleeding patients (model-based matched cohort). The third method, instead of matching, derived estimates based on regression modelling using the entire population (regression method). Three parallel analyses were conducted for the length of ICU stay attributable to clinically important bleeding.
Patients
A total of 1666 critically ill patients receiving mechanical ventilation for at least 48 hours.
Measurements
We prospectively collected data on patient demographics, APACHE II score, admitting diagnosis, daily MODS, clinically important bleeding, length of ICU stay, and mortality. Independent adjudicators determined the occurrence of clinically important gastrointestinal bleeding, defined as overt bleeding in association with haemodynamic compromise or blood transfusion.
Results
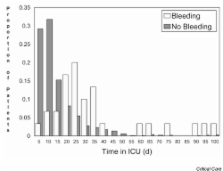
Of 1666 patients, 59 developed clinically important gastrointestinal bleeding. The mean APACHE II score was 22.9 ± 8.6 among bleeding patients and 23.3 ± 7.7 among non-bleeding patients. The risk of death was increased in patients with bleeding using all three analytic approaches (matched cohort method: relative risk [RR]= 2.9, 95% confidence interval (CI)= 1.6–5.5; model-based matched cohort method: RR = 1.8, 95% CI = 1.1–2.9; and the regression method: RR = 4.1, 95% CI = 2.6–6.5). However, this was not significant for the adjusted regression method (RR = 1.0, 95% CI = 0.6–1.7). The median length of ICU stay attributable to clinically important bleeding for these three methods, respectively, was 3.8 days (95% CI = -0.01 to 7.6 days), 6.7 days (95% CI = 2.7–10.7 days), and 7.9 days (95% CI = 1.4–14.4 days).
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome.
- Record: found
- Abstract: found
- Article: not found
Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay.
- Record: found
- Abstract: found
- Article: not found
