- Record: found
- Abstract: found
- Article: found
Long-term impact of a conditional cash transfer programme on maternal mortality: a nationwide analysis of Brazilian longitudinal data
Read this article at
Abstract
Background
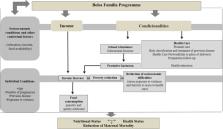
Reducing poverty and improving access to health care are two of the most effective actions to decrease maternal mortality, and conditional cash transfer (CCT) programmes act on both. The aim of this study was to evaluate the effects of one of the world’s largest CCT (the Brazilian Bolsa Familia Programme (BFP)) on maternal mortality during a period of 11 years.
Methods
The study had an ecological longitudinal design and used all 2548 Brazilian municipalities with vital statistics of adequate quality during 2004–2014. BFP municipal coverage was classified into four levels, from low to consolidated, and its duration effects were measured using the average municipal coverage of previous years. We used negative binomial multivariable regression models with fixed-effects specifications, adjusted for all relevant demographic, socioeconomic, and healthcare variables.
Results
BFP was significantly associated with reductions of maternal mortality proportionally to its levels of coverage and years of implementation, with a rate ratio (RR) reaching 0.88 (95%CI 0.81–0.95), 0.84 (0.75–0.96) and 0.83 (0.71–0.99) for intermediate, high and consolidated BFP coverage over the previous 11 years. The BFP duration effect was stronger among young mothers (RR 0.77; 95%CI 0.67–0.96). BFP was also associated with reductions in the proportion of pregnant women with no prenatal visits (RR 0.73; 95%CI 0.69–0.77), reductions in hospital case-fatality rate for delivery (RR 0.78; 95%CI 0.66–0.94) and increases in the proportion of deliveries in hospital (RR 1.05; 95%CI 1.04–1.07).
Conclusion
Our findings show that a consolidated and durable CCT coverage could decrease maternal mortality, and these long-term effects are stronger among poor mothers exposed to CCT during their childhood and adolescence, suggesting a CCT inter-generational effect. Sustained CCT coverage could reduce health inequalities and contribute to the achievement of the Sustainable Development Goal 3.1, and should be preserved during the current global economic crisis due to the COVID-19 pandemic.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: not found
Global causes of maternal death: a WHO systematic analysis.
- Record: found
- Abstract: found
- Article: not found