- Record: found
- Abstract: found
- Article: found
Clinical Significance of Perineal Descent in Pelvic Outlet Obstruction Diagnosed by using Defecography
Read this article at
Abstract
Purpose
The aim of this study was to evaluate the clinical significance of perineal descent (PD) in pelvic outlet obstruction patients diagnosed by using defecography.
Methods
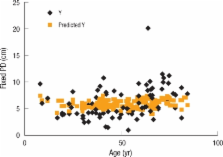
One hundred thirty-six patients with pelvic outlet obstruction (POO; median age 49 years) had more than one biofeedback session after defecography. Demographic finding, clinical bowel symptoms and anorectal physiological studies were compared for PD at rest and PD with dynamic changes.
Results
Age (r = 0.33; P < 0.001), rectocele diameter (r = 0.31; P < 0.01), symptoms of incontinence (P < 0.05) and number of vaginal deliveries (r = 0.46; P < 0.001) were correlated with increased fixed PD. However, the female gender (P < 0.005), rectal intussusceptions (P < 0.05), negative non-relaxing puborectalis syndrome (P < 0.00005) and rectocele (P < 0.0005) were correlated with increased dynamic PD. Duration of symptoms, number of bowel movements, history of pelvic surgery and difficult defecation were not related with PD. There was no significant correlation between fixed and dynamic PD and success of biofeedback therapy.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: not found
Sphincter denervation in anorectal incontinence and rectal prolapse.
- Record: found
- Abstract: found
- Article: not found