- Record: found
- Abstract: found
- Article: found
HIV incidence and factors associated with testing positive for HIV among men who have sex with men and transgender women in Myanmar: data from community‐based HIV testing services
Read this article at
Abstract
Introduction
In Myanmar, men who have sex with men (MSM) and transgender women (TW) are disproportionately affected by HIV, despite national HIV program scale‐up. However, limited HIV surveillance capacity prevents monitoring of epidemic trends and program impact. This study aimed to estimate HIV prevalence and incidence and explore associated sexual risk behaviours among MSM and TW clients attending HIV testing clinics in Myanmar.
Methods
An electronic data management system was implemented in two community‐based, MSM and TW ‐tailored HIV testing clinics in Myanmar in August 2016. Unique client identifiers enabled prospective monitoring of service engagement, testing frequency and outcomes. We estimated HIV incidence and rate of HIV diagnosis at baseline testing visit among clients over a 15 month period. Correlates of HIV diagnoses were identified using multivariable logistic regression.
Results
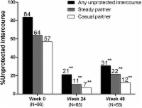
2794 MSM and TW were tested for HIV. At their baseline test, 38% of clients reported any previous testing and 93% reported being sexually active over the previous three months, with 74% reporting sex with casual male partners and 28% reporting consistent condom use with casual partners. 291 clients tested positive for HIV for the first time at baseline (10.4%; 95% CI: 9.3 to 11.6). Twelve incident cases were detected among 279 clients receiving ≥2 tests (incidence = 10.1 per 100 person‐years; 95% CI: 5.73 to 17.8). HIV diagnosis at baseline was significantly associated with being a transgender woman or a non‐openly disclosing man who has sex with men, age 26 to 39 years, and reporting no testing history.
Conclusions
High HIV incidence and new diagnoses being associated with reporting no testing history points to undiagnosed HIV driving transmissions in Myanmar. Repeat testing was uncommon. HIV programs in Myanmar must focus on promoting frequent HIV testing alongside adequate coverage of education and primary prevention interventions among MSM and TW.
Related collections
Most cited references23

- Record: found
- Abstract: found
- Article: found
Facilitators and barriers for retention in HIV care between testing and treatment in Asia—A study in Bangladesh, Indonesia, Lao, Nepal, Pakistan, Philippines and Vietnam
- Record: found
- Abstract: found
- Article: found