- Record: found
- Abstract: found
- Article: not found
The Effectiveness of High-Flow Nasal Cannula in Coronavirus Disease 2019 Pneumonia: A Retrospective Cohort Study
Read this article at
OBJECTIVES:
High-flow nasal cannula is widely used in acute hypoxemic respiratory failure due to coronavirus disease 2019, yet data regarding its effectiveness is lacking. More evidence is needed to guide patient selection, timing of high-flow nasal cannula initiation, and resource allocation. We aimed to assess time to discharge and time to death in severe coronavirus disease 2019 in patients treated with high-flow nasal cannula compared with matched controls. We also evaluated the ability of the respiratory rate-oxygenation ratio to predict progression to invasive mechanical ventilation.
DESIGN:
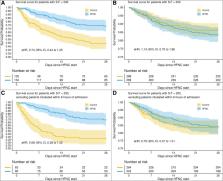
Time-dependent propensity score matching was used to create pairs of individuals who were then analyzed in a Cox proportional-hazards regression model to estimate high-flow nasal cannula’s effect on time to discharge and time to death. A secondary analysis excluded high-flow nasal cannula patients intubated within 6 hours of admission. A Cox proportional-hazards regression model was used to assess risk of invasive mechanical ventilation among high-flow nasal cannula patients stratified by respiratory rate-oxygenation.
PATIENTS:
All patients who were admitted with a laboratory-confirmed diagnosis of coronavirus disease 2019 were eligible for inclusion.
MEASUREMENTS AND MAIN RESULTS:
High-flow nasal cannula was associated with longer median time to discharge: 10.6 days (interquartile range, 7.1–15.8 d) versus 7.8 days (interquartile range, 4.9–12.1 d). Respiratory rate-oxygenation index performed poorly in predicting ventilation or death. In the primary analysis, there was no significant association between high-flow nasal cannula and hazard of death (adjusted hazard ratio, 0.79; 95% CI, 0.57–1.09). Excluding patients intubated within 6 hours of admission, high-flow nasal cannula was associated with reduced hazard of death (adjusted hazard ratio, 0.67; 95% CI, 0.45–0.99).
CONCLUSIONS:
Among unselected patients with severe coronavirus disease 2019 pneumonia, high-flow nasal cannula was not associated with a statistically significant reduction in hazard of death. However, in patients not mechanically ventilated within 6 hours of admission, high-flow nasal cannula was associated with a significantly reduced hazard of death.
Related collections
Most cited references36
- Record: found
- Abstract: not found
- Article: not found
mice: Multivariate Imputation by Chained Equations inR
- Record: found
- Abstract: found
- Article: not found
Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries.
- Record: found
- Abstract: not found
- Article: not found
