- Record: found
- Abstract: found
- Article: found
Pneumococcal and influenza immunization in asplenic persons: a retrospective population-based cohort study 1990-2002
Read this article at
Abstract
Background
Splenectomy is associated with increased risk for bacteremia, due to impaired clearance of bloodborne agents and to altered phagocytosis and humoral immunity. We conducted a retrospective cohort study of patients at risk for splenectomy for a 13-year period to determine immunization coverage, and outcomes of those with and without splenectomy, and with or without receipt of influenza or pneumococcal vaccine.
Methods
Data were extracted from the provincial Medical Services Insurance database for insured services rendered by a physician for 1990-2002, and from the Vital Statistics Death database. The eligible cohort was selected based on diagnostic codes for hematologic conditions for which splenectomy might be considered, such as immune thrombocytopenia. Each patient was followed longitudinally from the date of first diagnosis until 31Dec2002, or death, or relocation out-of province. In addition, persons with splenectomy and no hematologic condition were identified and followed for 6 months post-surgery. Infectious illness rates per 100 person-years of observation and death rates were calculated with and without splenectomy. Death rates were determined using splenectomy status as a time-dependent covariate. The relationship between splenectomy and death according to immunization status was examined using Cox proportional hazard ratios.
Results
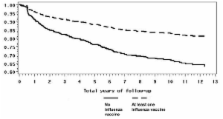
Of 38,812 persons in the cohort 427 subjects with a hematologic diagnosis had splenectomy and another 452 subjects without a hematologic diagnosis had this surgery. 72% were > 18 years of age. Pneumococcal immunization was recorded in 16.5% of asplenic patients overall, and was not associated with reduced risk of death in these persons (adjusted Hazard Ratio [HR] = 1.07, 95% CI 0.70 - 1.65). Influenza immunization was recorded in 53.1% of asplenic patients overall, and was associated with reduced risk of death (adjusted HR = 0.46, 0.33-0.62). No pneumococcal or influenza immunization was recorded in patients with a hematologic diagnosis without splenectomy. Infectious illness visits were higher among all patients who had a splenectomy than among those without a splenectomy (151 visits/100 person-years of observation in the post-splenectomy period vs. 120 visits/100 person-years; p < 0.0001).
Conclusions
In asplenic patients, influenza immunization is associated with a 54% reduced risk of death compared to unimmunized asplenic persons; no reduction in risk was demonstrated with (polysaccharide) pneumococcal vaccine. Vaccine coverage in the entire cohort was less than routinely recommended. Improved delivery of infection prevention programs to this population is warranted. Conjugate pneumococcal vaccines should be urgently studied in this immunocompromised population.
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
Direct and indirect effects of routine vaccination of children with 7-valent pneumococcal conjugate vaccine on incidence of invasive pneumococcal disease--United States, 1998-2003.
- Record: found
- Abstract: found
- Article: not found
Risk of infection and death among post-splenectomy patients.
- Record: found
- Abstract: found
- Article: not found