- Record: found
- Abstract: found
- Article: found
Does the distance to the cancer center affect psycho-oncological care and emergency visits of patients with IDH wild-type gliomas? A retrospective study
Read this article at
Abstract
Background
Malignant isocitrate dehydrogenase wild-type (IDHwt) gliomas impose a high symptomatic and psychological burden. Wide distances from patients’ homes to cancer centers may affect the delivery of psycho-oncological care. Here, we investigated, in a large brain tumor center with a rural outreach, the initiation of psycho-oncological care depending on spatial distance and impact of psycho-oncological care on emergency visits.
Methods
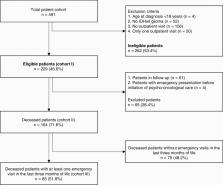
Electronic patient charts, the regional tumor registry, and interviews with the primary care physicians were used to investigate clinical data, psycho-oncological care, and emergency unit visits. Interrelations with socio-demographic, clinical, and treatment aspects were investigated using univariable and multivariable binary logistic regression analysis and the Pearson’s Chi-square test.
Results
Of 491, 229 adult patients of this retrospective cohort fulfilled the inclusion criteria for analysis. During the last three months of their lives, 48.9% received at least one psycho-oncological consultation, and 37.1% visited the emergency unit at least once. The distance from the cancer center did neither affect the initiation of psycho-oncological care nor the rate of emergency unit visits. Receiving psycho-oncological care did not correlate with the frequency of emergency unit visits in the last three months of life.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: found
The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary.
- Record: found
- Abstract: found
- Article: not found
Symptom Monitoring With Patient-Reported Outcomes During Routine Cancer Treatment: A Randomized Controlled Trial.
- Record: found
- Abstract: found
- Article: not found