- Record: found
- Abstract: found
- Article: found
Extended resection including adjacent organs and Ki-67 labeling index are prognostic factors in patients with retroperitoneal soft tissue sarcomas
Read this article at
Abstract
Background
Because retroperitoneal soft tissue sarcomas (RPS) are extremely rare, there is a significant lack of clinicopathologic information to optimize the treatment strategy. The aim of this study was to evaluate the prognostic factors in RPS, with particular focus on the Ki-67 labeling index (LI).
Methods
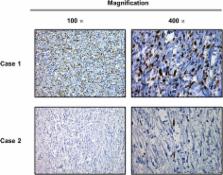
We included the data from a total of 23 patients who received treatment for primary RPS at a single center. The variables analyzed in this study included tumor size, histological type, malignancy grade, necrosis, mitosis, and Ki-67 LI. Kaplan-Meier and Cox proportional regression analyses of overall survival (OS) were performed to identify significant prognostic variables.
Results
Of the 23 patients who underwent surgical resection, 9 (39 %) underwent simple resection of the tumor and 14 (61 %) extended resection including the adjacent organs. In the univariate analysis, a simple tumor resection and a high Ki-67 LI were associated with shorter OS. The multivariate analysis revealed that simple tumor resection and a high Ki-67 LI were independent negative prognostic factors for OS.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Primary retroperitoneal sarcomas: a multivariate analysis of surgical factors associated with local control.
- Record: found
- Abstract: found
- Article: not found
Prognostic factors in retroperitoneal sarcoma: a multivariate analysis of a series of 165 patients of the French Cancer Center Federation Sarcoma Group.
- Record: found
- Abstract: found
- Article: not found