- Record: found
- Abstract: found
- Article: found
Spontaneous pneumomediastinum in a healthy young female: A case report and literature review
Read this article at
Abstract
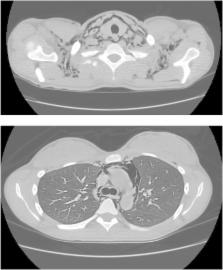
Spontaneous pneumomediastinum (SPM) is an uncommon finding in young adults presenting usually without any comorbidities or an underlying pathology. It is most commonly due to alveolar rupture in the setting of an inciting event such an underlying asthma, barotrauma, valsalva maneuver, or esophageal rupture. Individuals can have varying presentations, from chest pain, dyspnea and dysphagia, to anxiety, weakness, or facial and neck swelling. The majority of patients have subcutaneous emphysema on examination and can have abnormal laboratory findings such as an elevated C-reactive proteins and leukocytosis. Diagnostic modalities used include chest x-ray, CT scan, ultrasound and barium swallow or esophagram. Majority of individuals and treated conservatively with rest, analgesia and oxygen administration. The prognosis of SPM is usually good with resolution within several days in most cases and the recurrence rate is very low. We report the case of a 22-year-old female presented with SPM diagnosed by chest x-ray and chest CT scan who was treated conservatively with subsequent spontaneous resolution.
Related collections
Most cited references13
- Record: found
- Abstract: found
- Article: found
Spontaneous Pneumomediastinum: Time for Consensus
- Record: found
- Abstract: found
- Article: not found
Spontaneous pneumomediastinum: a benign curiosity or a significant problem?
- Record: found
- Abstract: found
- Article: not found