- Record: found
- Abstract: found
- Article: found
A review of -multidrug-resistant Enterobacteriaceae in a neonatal unit in Johannesburg, South Africa
Read this article at
Abstract
Aim
This study aimed to review neonatal sepsis caused by multi-drug resistant Enterobacteriaceae (MDRE) in neonates in Johannesburg, South Africa.
Methods
This was a cross sectional retrospective review of MDRE in neonates admitted to a tertiary neonatal unit between 1 January 2013 and 31 December 2015.
Results
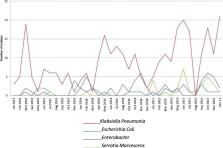
There were 465 infections in 291 neonates. 68.6% were very low birth weight (< 1500 g). The median age of infection was 14.0 days. Risk factors for MDRE included prematurity ( p = 0.01), lower birth weight ( p = 0.04), maternal HIV infection ( p = 0.02) and oxygen on day 28 ( p < 0.001). The most common isolate was Klebsiella pneumoniae (66.2%). Total MDRE isolates increased from 0.39 per 1000 neonatal admissions in 2013 to 1.4 per 1000 neonatal admissions in 2015 ( p < 0.001). There was an increase in carbapenem-resistant Enterobacteriaceae (CRE) from 2.6% in 2013 to 8.9% in 2015 ( p = 0.06). Most of the CRE were New Delhi metallo—β lactamase- (NDM) producers.
The all-cause mortality rate was 33.3%. Birth weight ( p = 0.003), necrotising enterocolitis ( p < 0.001) and mechanical ventilation ( p = 0.007) were significantly associated with mortality. Serratia marcescens was isolated in 55.2% of neonates that died.
Conclusions
There was a significant increase in MDRE in neonatal sepsis during the study period, with the emergence of CRE. This confirms the urgent need to intensify antimicrobial stewardship efforts and address infection control and prevention in neonatal units in LMICs. Overuse of broad- spectrum antibiotics should be prevented.
Related collections
Most cited references20
- Record: found
- Abstract: found
- Article: not found
Risk factors and outcomes for multidrug-resistant Gram-negative bacteremia in the NICU.
- Record: found
- Abstract: found
- Article: not found
Extended-spectrum β-lactamase-producing Enterobacteriaceae in children: old foe, emerging threat.
- Record: found
- Abstract: found
- Article: not found