- Record: found
- Abstract: found
- Article: not found
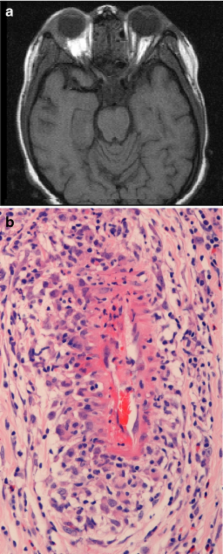
Small vessel vasculitis
Read this article at
Abstract
The pediatric small vessel vasculitides reviewed in this article are Henoch–Schönlein purpura (HSP) and the anti-neutrophil cytoplasmic antibody-associated vasculitides (AAV). The new classification criteria for HSP and Wegener’s granulomatosis are now validated and will facilitate the conduct of future epidemiological studies and clinical trials. The clinical manifestations of small vessel vasculitis in children are described, and current therapies discussed. There is a lack of good clinical trial data on which to base therapy for HSP. Similarly, data based on randomized controlled trials (RCTs) for pediatric AAV are lacking, although children with AAV are for the first time now included in a RCT of mycophenolate mofetil versus cyclophosphamide. Significant challenges remain in the field of pediatric small vessel vasculitis, including the development of validated disease outcome measures and biomarkers to be used in clinical trials. Lastly, long-term outcome data are lacking in survivors of pediatric small vessel vasculitis.
Related collections
Most cited references57
- Record: found
- Abstract: found
- Article: not found
Trimethoprim-sulfamethoxazole (co-trimoxazole) for the prevention of relapses of Wegener's granulomatosis. Dutch Co-Trimoxazole Wegener Study Group.
- Record: found
- Abstract: found
- Article: not found
Antineutrophil cytoplasmic autoantibodies specific for myeloperoxidase cause glomerulonephritis and vasculitis in mice.
- Record: found
- Abstract: not found
- Article: not found
