- Record: found
- Abstract: found
- Article: found
Small incision lenticule extraction (SMILE) history, fundamentals of a new refractive surgery technique and clinical outcomes
Read this article at
Abstract
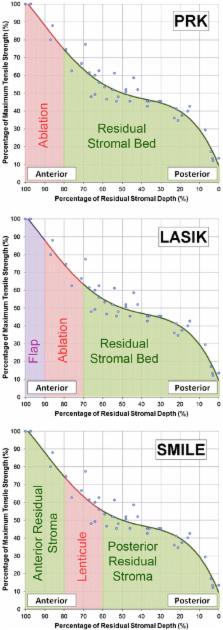
This review summarizes the current status of the small incision lenticule extraction (SMILE) procedure. Following the early work by Sekundo et al. and Shah et al., SMILE has become increasingly popular. The accuracy of the creation of the lenticule with the VisuMax femtosecond laser (Carl Zeiss Meditec) has been verified using very high-frequency (VHF) digital ultrasound and optical coherence tomography (OCT). Visual and refractive outcomes have been shown to be similar to those achieved with laser in situ keratomileusis (LASIK), notably in a large population reported by Hjortdal, Vestergaard et al. Safety in terms of the change in corrected distance visual acuity (CDVA) has also been shown to be similar to LASIK. It was expected that there would be less postoperative dry eye after SMILE compared to LASIK because the anterior stroma is disturbed only by the small incision, meaning that the anterior corneal nerves should be less affected. A number of studies have demonstrated a lower reduction and faster recovery of corneal sensation after SMILE than LASIK. Some studies have also used confocal microscopy to demonstrate a lower decrease in subbasal nerve fiber density after SMILE than LASIK. The potential biomechanical advantages of SMILE have been modeled by Reinstein et al. based on the non-linearity of tensile strength through the stroma. Studies have reported a similar change in Ocular Response Analyzer (Reichert) parameters after SMILE and LASIK, however, these have previously been shown to be unreliable as a representation of corneal biomechanics. Retreatment options after SMILE are discussed. Tissue addition applications of the SMILE procedure are also discussed including the potential for cryo-preservation of the lenticule for later reimplantation (Mohamed-Noriega, Angunawela, Lim et al.), and a new procedure referred to as endokeratophakia in which a myopic SMILE lenticule is implanted into a hyperopic patient (Pradhan et al.). Finally, studies reporting microdistortions in Bowman’s layer and corneal wound healing responses are also described.
Additional non-English abstract (French, Francais)
Cette revue résume les connaissances actuelles sur la procedure SMILE (small incision lenticule extraction). Apres les travaux préliminaires des groupes de Sekundo et al. et de Shah et al., la procedure SMILE est désormais devenue courante. Le laser femtosecond VisuMax (Carl Zeiss Meditec) permet une découpe précise du lenticule, comme cela a été vérifié par ultrasound numérique à tres haute fréquence (Artemis) et par OCT. Il a été démontré, entre autres par Hjortdal, Vestergaard, et al. dans leur etude sur une population large, que les résultats visuels et refractifs sont comparables à ceux du LASIK, et que le risque de perte de lignes d’acuité corrigée est aussi semblable à celui du LASIK. Avec SMILE, contrairement au LASIK, la partie antérieure du stroma étant seulement découpée par une incision de petite taille, les nerfs cornéens antérieurs sont moins touchés et par consequent, le taux d’yeux secs en phase post-opératoire devrait etre plus faible après SMILE qu’apres LASIK. Quelques études ont effectivement démontré que la sensation cornéenne était moins réduite après SMILE qu’après LASIK et que la récupération de la sensation cornéenne était plus rapide. Quelques études ont aussi utilisé la microscopie confocale pour prouver qu’il y avait une diminution plus faible de la densité des fibres nerveuses de la couche sub-basale après SMILE qu’apres LASIK. Au niveau biomécanique, Reinstein et al. ont proposé un modèle basé sur la non-linéarité de la force de tension du stroma, mettant en avant les avantages potentiels de SMILE. Certaines études ont comparé les paramètres mesurés par l’Ocular Response Analayzer (Reichert) et rapporté un changement similaire après SMILE ou LASIK; cependant, on sait que ces paramètres ne peuvent pas etre pris en compte pour représenter la biomécanique cornéenne. Les options de re-traitement après SMILE sont présentées, ainsi que la possibilité d’ajouter du tisuu cornéen: par example, le potential de cryo-preservation du lenticule pour une ré-implantation ultérieure (Mohamed-Noriega, Angunawela, Lim et al.), et une nouvelle procedure nommée endokératophakie dans laquelle un lenticule SMILE est implanté dans la cornée d’un oeil hypermétrope (Pradhan et al.). Pour finir, des études rapportant des micro-distortions dans la couche de Bowmans et des études sur le processus de reparation de la cornée sont décrites.
Related collections
Most cited references83
- Record: found
- Abstract: found
- Article: not found
Results of small incision lenticule extraction: All-in-one femtosecond laser refractive surgery.
- Record: found
- Abstract: found
- Article: not found
Safety and complications of more than 1500 small-incision lenticule extraction procedures.
- Record: found
- Abstract: found
- Article: not found