- Record: found
- Abstract: found
- Article: found
What works in implementation of integrated care programs for older adults with complex needs? A realist review
Read this article at
Abstract
Purpose
A realist review of the evaluative evidence was conducted on integrated care (IC) programs for older adults to identify key processes that lead to the success or failure of these programs in achieving outcomes such as reduced healthcare utilization, improved patient health, and improved patient and caregiver experience.
Data sources
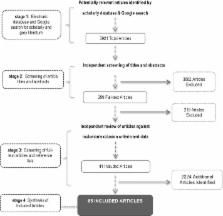
International academic literature was searched in 12 indexed, electronic databases and gray literature through internet searches, to identify evaluative studies.
Study selection
Inclusion criteria included evaluative literature on integrated, long-stay health and social care programs, published between January 1980 and July 2015, in English.
Data extraction
Data were extracted on the study purpose, period, setting, design, population, sample size, outcomes, and study results, as well as explanations of mechanisms and contextual factors influencing outcomes.
Results of data synthesis
A total of 65 articles, representing 28 IC programs, were included in the review. Two context-mechanism-outcome configurations (CMOcs) were identified: (i) trusting multidisciplinary team relationships and (ii) provider commitment to and understanding of the model. Contextual factors such as strong leadership that sets clear goals and establishes an organizational culture in support of the program, along with joint governance structures, supported team collaboration and subsequent successful implementation. Furthermore, time to build an infrastructure to implement and flexibility in implementation, emerged as key processes instrumental to success of these programs.
Related collections
Most cited references54
- Record: found
- Abstract: found
- Article: not found
Integrated care programmes for chronically ill patients: a review of systematic reviews.
- Record: found
- Abstract: found
- Article: not found
What fosters or prevents interprofessional teamworking in primary and community care? A literature review.
- Record: found
- Abstract: found
- Article: not found