- Record: found
- Abstract: found
- Article: found
Clinical relevance of pulse pressure variations for predicting fluid responsiveness in mechanically ventilated intensive care unit patients: the grey zone approach

Read this article at
Abstract
Introduction
Pulse pressure variation (PPV) has been shown to predict fluid responsiveness in ventilated intensive care unit (ICU) patients. The present study was aimed at assessing the diagnostic accuracy of PPV for prediction of fluid responsiveness by using the grey zone approach in a large population.
Methods
The study pooled data of 556 patients from nine French ICUs. Hemodynamic (PPV, central venous pressure (CVP) and cardiac output) and ventilator variables were recorded. Responders were defined as patients increasing their stroke volume more than or equal to 15% after fluid challenge. The receiver operating characteristic (ROC) curve and grey zone were defined for PPV. The grey zone was evaluated according to the risk of fluid infusion in hypoxemic patients.
Results
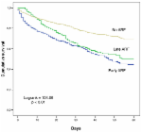
Fluid challenge led to increased stroke volume more than or equal to 15% in 267 patients (48%). The areas under the ROC curve of PPV and CVP were 0.73 (95% confidence interval (CI): 0.68 to 0.77) and 0.64 (95% CI 0.59 to 0.70), respectively ( P <0.001). A grey zone of 4 to 17% (62% of patients) was found for PPV. A tidal volume more than or equal to 8 ml.kg −1 and a driving pressure (plateau pressure - PEEP) more than 20 cmH 2O significantly improved the area under the ROC curve for PPV. When taking into account the risk of fluid infusion, the grey zone for PPV was 2 to 13%.
Related collections
Most cited references40
- Record: found
- Abstract: found
- Article: not found
A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study.
- Record: found
- Abstract: found
- Article: not found
Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature.
- Record: found
- Abstract: found
- Article: found