- Record: found
- Abstract: found
- Article: found
Assessment of SARS-CoV-2 Screening Strategies to Permit the Safe Reopening of College Campuses in the United States
Read this article at
Key Points
Question
What screening and isolation programs for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will keep students at US residential colleges safe and permit the reopening of campuses?
Findings
This analytic modeling study of a hypothetical cohort of 4990 college-age students without SARS-CoV-2 infection and 10 students with undetected asymptomatic cases of SARS-CoV-2 infection suggested that frequent screening (every 2 days) of all students with a low-sensitivity, high-specificity test might be required to control outbreaks with manageable isolation dormitory utilization at a justifiable cost.
Abstract
This analytic modeling study defines the screening performance standards for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) tests that would permit the safe return of students to US residential college campuses for the fall 2020 semester.
Abstract
Importance
The coronavirus disease 2019 (COVID-19) pandemic poses an existential threat to many US residential colleges; either they open their doors to students in September or they risk serious financial consequences.
Objective
To define severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) screening performance standards that would permit the safe return of students to US residential college campuses for the fall 2020 semester.
Design, Setting, and Participants
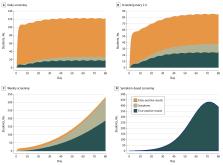
This analytic modeling study included a hypothetical cohort of 4990 students without SARS-CoV-2 infection and 10 with undetected, asymptomatic SARS-CoV-2 infection at the start of the semester. The decision and cost-effectiveness analyses were linked to a compartmental epidemic model to evaluate symptom-based screening and tests of varying frequency (ie, every 1, 2, 3, and 7 days), sensitivity (ie, 70%-99%), specificity (ie, 98%-99.7%), and cost (ie, $10/test-$50/test). Reproductive numbers (R t) were 1.5, 2.5, and 3.5, defining 3 epidemic scenarios, with additional infections imported via exogenous shocks. The model assumed a symptomatic case fatality risk of 0.05% and a 30% probability that infection would eventually lead to observable COVID-19–defining symptoms in the cohort. Model projections were for an 80-day, abbreviated fall 2020 semester. This study adhered to US government guidance for parameterization data.
Main Outcomes and Measures
Cumulative tests, infections, and costs; daily isolation dormitory census; incremental cost-effectiveness; and budget impact.
Results
At the start of the semester, the hypothetical cohort of 5000 students included 4990 (99.8%) with no SARS-CoV-2 infection and 10 (0.2%) with SARS-CoV-2 infection. Assuming an R t of 2.5 and daily screening with 70% sensitivity, a test with 98% specificity yielded 162 cumulative student infections and a mean isolation dormitory daily census of 116, with 21 students (18%) with true-positive results. Screening every 2 days resulted in 243 cumulative infections and a mean daily isolation census of 76, with 28 students (37%) with true-positive results. Screening every 7 days resulted in 1840 cumulative infections and a mean daily isolation census of 121 students, with 108 students (90%) with true-positive results. Across all scenarios, test frequency was more strongly associated with cumulative infection than test sensitivity. This model did not identify symptom-based screening alone as sufficient to contain an outbreak under any of the scenarios we considered. Cost-effectiveness analysis selected screening with a test with 70% sensitivity every 2, 1, or 7 days as the preferred strategy for an R t of 2.5, 3.5, or 1.5, respectively, implying screening costs of $470, $910, or $120, respectively, per student per semester.
Conclusions and Relevance
In this analytic modeling study, screening every 2 days using a rapid, inexpensive, and even poorly sensitive (>70%) test, coupled with strict behavioral interventions to keep R t less than 2.5, is estimated to maintain a controllable number of COVID-19 infections and permit the safe return of students to campus.
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia
- Record: found
- Abstract: found
- Article: not found
The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application
- Record: found
- Abstract: found
- Article: not found
Temporal dynamics in viral shedding and transmissibility of COVID-19
Author and article information
Comments
Comment on this article
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.