- Record: found
- Abstract: found
- Article: found
MYC rearrangement but not extra MYC copies is an independent prognostic factor in patients with mantle cell lymphoma
Read this article at
Abstract
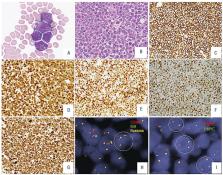
Mantle cell lymphoma (MCL) with MYC rearrangement ( MYC-R) is rare and little is known about the importance of MYC extra copies (EC) in the absence of MYC-R in MCL patients. This study includes 88 MCL patients with MYC tested by fluorescence in situ hybridization and/or conventional cytogenetics, including 27 with MYC-R, 21 with MYC-EC, and 40 with normal MYC-NL. MCL patients with MYC-R more often had blastoid/pleomorphic morphology; a higher frequency of CD10, MYC, and simultaneous MYC and BCL2 expression; a higher level of MYC; and a higher Ki67 proliferation rate ( P<0.05) than those without MYC-R. Although patients with MYC-R more frequently received intensive chemotherapy ( P=0.001), their overall survival (OS) was significantly shorter than those without MYC-R. Compared with patients with MYC/BCL2 double-hit lymphoma (DHL), patients with MYC-R MCL had a similar OS but more commonly had bone marrow involvement, Ann Arbor stage IV disease, and a different immunophenotype. MCL patients with MYC-EC showed an OS intermediate between those with MYC-R and MYC-NL, either all or only blastoid/pleomorphic MCL patients included. Multivariate analysis showed that MYC-R, but not MYC-EC, had an independent and negative impact on OS. In conclusion, MYC-R but not MYC-EC showed a higher MYC expression and is an adverse prognostic factor for MCL patients. Although the OS of MCL patients with MYC-R is similar to that of MYC/BCL2DHL patients, these groups have different clinicopathologic features supporting the retention of MCL with MYC-R in the category of MCL, as recommended in the revised World Health Organization classification.
Related collections
Most cited references47
- Record: found
- Abstract: found
- Article: not found
Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray.
- Record: found
- Abstract: found
- Article: not found
A new prognostic index (MIPI) for patients with advanced-stage mantle cell lymphoma.
- Record: found
- Abstract: found
- Article: not found