- Record: found
- Abstract: found
- Article: found
The Magnitude of MTB and Rifampicin Resistance MTB Using Xpert-MTB/RIF Assay Among Tuberculosis Suspected Patients in Gedeo Zone, Southern Ethiopia
Read this article at
Abstract
Background
Tuberculosis (TB) remains a major global health problem causing death among millions of people each year. The new barrier that challenges the control of tuberculosis is the emerging and the increasing number of drug-resistant TB that becomes a world concern. This study aimed to determine the magnitude of rifampicin-resistant Mycobacterium tuberculosis (RR-MTB) among presumptive TB patients attending Dilla University Referral Hospital, Gedeo Zone, Ethiopia.
Methods
A retrospective cross-sectional study was conducted at Dilla University Referral Hospital from January 2014 to December 2020. Sputum results were done using Xpert MTB/RIF assay and other necessary data were collected from the registration logbooks using a standardized data extraction format and analyzed using SPSS version 23 statistical software.
Results
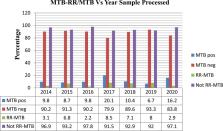
A total of 17,745 presumptive TB patients were included, of which 62.2% were males. The overall prevalence of Mycobacterium tuberculosis (MTB) was 11.8%, of which 5.1% were confirmed to have RR-MTB. Extra-pulmonary TB was reported in 1.5% of the study participants. The highest prevalence of MTB and RR-MTB was recorded in 2017 with a prevalence of 20.1% and 8.5%, respectively. All age groups were significantly associated with a higher prevalence of MTB ( p < 0.036). TB patients with a history of previous treatment and HIV positive were significantly associated with MTB ( P < 0.021), while RR-MTB was only significantly associated with patients with a history of previous treatment ( P < 0.018).
Conclusion
A high magnitude of MTB and RR-MTB was reported among TB patients with HIV and a history of previous treatment. Therefore, coordinated efforts should be applied to the improvement of treatment adherence of known TB cases, and appropriate control and prevention methods to reduce the emergence and increase of MTB and RR-MTB cases.
Related collections
Most cited references52
- Record: found
- Abstract: not found
- Article: not found
WHO's new end TB strategy.
- Record: found
- Abstract: found
- Article: not found