- Record: found
- Abstract: found
- Article: found
Associations of tobacco smoking with body mass distribution; a population-based study of 65,875 men and women in midlife
Read this article at
Abstract
Background
Studies indicate an effect of smoking toward abdominal obesity, but few assess hip and waist circumferences (HC and WC) independently. The present study aimed to assess the associations of smoking status and volume smoked with HC and WC and their ratio in a population with low prevalence of obesity together with high prevalence of smoking.
Methods
We used cross-sectional survey data from 11 of a total 19 Norwegian counties examined in 1997–99 including 65,875 men and women aged 39–44 years. Analysis of associations were adjusted for confounding by socioeconomic position, health indicators, and additionally for BMI.
Results
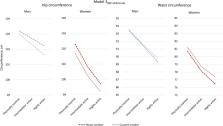
Compared with never-smokers, when adjusting for confounders and in addition for BMI, mean HC remained lower while mean WC and waist-hip-ratio (WHR) were higher in current smokers. The finding of a lower HC and higher WHR level among smokers was consistent by sex and in strata by levels of education and physical activity, while the finding of higher WC by smoking was less consistent. Among current smokers, BMI-adjusted mean HC decreased whereas WC and WHR increased by volume smoked. Compared with current smokers, former smokers had higher BMI-adjusted HC, lower WHR and among women WC was lower.
Conclusions
The main finding in this study was the consistent negative associations of smoking with HC. In line with the hypothesis that lower percentage gluteofemoral fat is linked with higher cardiovascular risk, our results suggest that smoking impacts cardiovascular risk through mechanisms that reduce the capacity of fat storage in the lower body region.
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: found
Body mass index, waist circumference and waist-hip ratio: which is the better discriminator of cardiovascular disease mortality risk? Evidence from an individual-participant meta-analysis of 82 864 participants from nine cohort studies : Adiposity & mortality
- Record: found
- Abstract: found
- Article: not found
Health consequences of smoking 1-4 cigarettes per day.
- Record: found
- Abstract: found
- Article: not found