- Record: found
- Abstract: found
- Article: found
Evaluating glaucomatous abnormality in peripapillary optical coherence tomography enface visualisation of the retinal nerve fibre layer reflectance
Read this article at
Abstract
Purpose
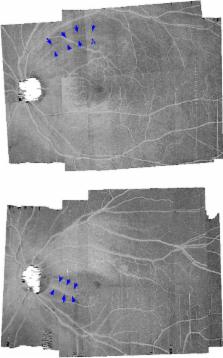
Optical coherence tomography ( OCT) enface visualisation of the retinal nerve fibre layer ( RNFL) reflectance has been found to have some advantages over retinal thickness measures. However, it is not yet clear how abnormalities on enface images relate to findings of abnormalities from other clinical measures such as the circumpapillary retinal nerve fibre layer thickness ( cRNFLT). We developed a technique to analyse the RNFL reflectance on the OCT enface images, and to investigate its relation with the cRNFLT.
Methods
Spectralis ( http://www.heidelbergengineering.com) OCT scans of the central retinal ±24° were analysed in the study eye of 31 controls and 33 patients, ages 61 (±9) and 69 (±8) years respectively. Enface slab‐images were extracted at 16–24, 24–36, and 24–52 μm from the inner limiting membrane in the temporal raphe, perifoveal and disc regions respectively. Reflectance probability maps were generated for the patients based on the control data. Glaucomatous abnormality was defined on the slab‐images when the slab‐area with reflectance abnormality was greater than the 95th percentile, and on the cRNFLT when the thickness measure was less than the fifth percentile, of that found in controls. The fraction of slab‐image showing reflectance abnormality was compared to cRNFLT in the patient group, using Spearman's rho. Agreement between the findings of abnormality based on cRNFLT and slab‐image reflectance was assessed using Cohen's kappa.
Results
Slab‐image and cRNFLT findings were in agreement for 26/33 eyes; four subjects showed cRNFLT abnormality but not slab‐image abnormality, and three subjects showed slab‐image abnormality but not cRNFLT abnormality. Spearman's rho found r s(31) = −0.82. The reflectance findings and cRNFLT findings were consistent in 27/33 for both the superior temporal ( ST) and inferior temporal ( IT) sectors, and Cohen's kappa found 0.53 and 0.61 respectively.
Conclusion
The surface area of enface slab‐images showing RNFL reflectance were strongly related to the cRNFLT measures, and the classification of a subject with glaucoma based on enface reflectance findings and cRNFLT findings had a generally good agreement. The larger retinal area assessed by the enface method preserves the spatial location of the RNFL abnormalities, and makes the technique a useful approach for identifying regions of potential RNFL abnormality for targeted perimetry.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Morphologic changes in the lamina cribrosa correlated with neural loss in open-angle glaucoma.
- Record: found
- Abstract: found
- Article: not found
Shadow removal and contrast enhancement in optical coherence tomography images of the human optic nerve head.
- Record: found
- Abstract: found
- Article: not found