- Record: found
- Abstract: found
- Article: not found
Comorbidity and its Impact on Patients with COVID-19
Read this article at
Abstract
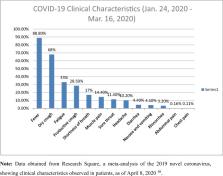
A novel human coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was identified in Wuhan, China, in December 2019. Since then, the virus has made its way across the globe to affect over 180 countries. SARS-CoV-2 has infected humans in all age groups, of all ethnicities, both males and females while spreading through communities at an alarming rate. Given the nature of this virus, there is much still to be learned; however, we know that the clinical manifestations range from a common cold to more severe diseases such as bronchitis, pneumonia, severe acute respiratory distress syndrome (ARDS), multi-organ failure, and even death. It is believed that COVID-19, in those with underlying health conditions or comorbidities, has an increasingly rapid and severe progression, often leading to death. This paper examined the comorbid conditions, the progression of the disease, and mortality rates in patients of all ages, infected with the ongoing COVID-19 disease. An electronic literature review search was performed, and applicable data was then collected from peer-reviewed articles published from January to April 20, 2020. From what is known at the moment, patients with COVID-19 disease who have comorbidities, such as hypertension or diabetes mellitus, are more likely to develop a more severe course and progression of the disease. Furthermore, older patients, especially those 65 years old and above who have comorbidities and are infected, have an increased admission rate into the intensive care unit (ICU) and mortality from the COVID-19 disease. Patients with comorbidities should take all necessary precautions to avoid getting infected with SARS CoV-2, as they usually have the worst prognosis.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China
- Record: found
- Abstract: found
- Article: not found
Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study
- Record: found
- Abstract: found
- Article: not found
