- Record: found
- Abstract: found
- Article: found
Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in children younger than 5 years in 2019: a systematic analysis
Read this article at
Summary
Background
Respiratory syncytial virus (RSV) is the most common cause of acute lower respiratory infection in young children. We previously estimated that in 2015, 33·1 million episodes of RSV-associated acute lower respiratory infection occurred in children aged 0–60 months, resulting in a total of 118 200 deaths worldwide. Since then, several community surveillance studies have been done to obtain a more precise estimation of RSV associated community deaths. We aimed to update RSV-associated acute lower respiratory infection morbidity and mortality at global, regional, and national levels in children aged 0–60 months for 2019, with focus on overall mortality and narrower infant age groups that are targeted by RSV prophylactics in development.
Methods
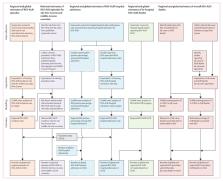
In this systematic analysis, we expanded our global RSV disease burden dataset by obtaining new data from an updated search for papers published between Jan 1, 2017, and Dec 31, 2020, from MEDLINE, Embase, Global Health, CINAHL, Web of Science, LILACS, OpenGrey, CNKI, Wanfang, and ChongqingVIP. We also included unpublished data from RSV GEN collaborators. Eligible studies reported data for children aged 0–60 months with RSV as primary infection with acute lower respiratory infection in community settings, or acute lower respiratory infection necessitating hospital admission; reported data for at least 12 consecutive months, except for in-hospital case fatality ratio (CFR) or for where RSV seasonality is well-defined; and reported incidence rate, hospital admission rate, RSV positive proportion in acute lower respiratory infection hospital admission, or in-hospital CFR. Studies were excluded if case definition was not clearly defined or not consistently applied, RSV infection was not laboratory confirmed or based on serology alone, or if the report included fewer than 50 cases of acute lower respiratory infection. We applied a generalised linear mixed-effects model (GLMM) to estimate RSV-associated acute lower respiratory infection incidence, hospital admission, and in-hospital mortality both globally and regionally (by country development status and by World Bank Income Classification) in 2019. We estimated country-level RSV-associated acute lower respiratory infection incidence through a risk-factor based model. We developed new models (through GLMM) that incorporated the latest RSV community mortality data for estimating overall RSV mortality. This review was registered in PROSPERO (CRD42021252400).
Findings
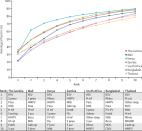
In addition to 317 studies included in our previous review, we identified and included 113 new eligible studies and unpublished data from 51 studies, for a total of 481 studies. We estimated that globally in 2019, there were 33·0 million RSV-associated acute lower respiratory infection episodes (uncertainty range [UR] 25·4–44·6 million), 3·6 million RSV-associated acute lower respiratory infection hospital admissions (2·9–4·6 million), 26 300 RSV-associated acute lower respiratory infection in-hospital deaths (15 100–49 100), and 101 400 RSV-attributable overall deaths (84 500–125 200) in children aged 0–60 months. In infants aged 0–6 months, we estimated that there were 6·6 million RSV-associated acute lower respiratory infection episodes (4·6–9·7 million), 1·4 million RSV-associated acute lower respiratory infection hospital admissions (1·0–2·0 million), 13 300 RSV-associated acute lower respiratory infection inhospital deaths (6800–28 100), and 45700 RSV-attributable overall deaths (38 400–55 900). 2·0% of deaths in children aged 0–60 months (UR 1·6–2·4) and 3·6% of deaths in children aged 28 days to 6 months (3·0–4·4) were attributable to RSV. More than 95% of RSV-associated acute lower respiratory infection episodes and more than 97% of RSV-attributable deaths across all age bands were in low-income and middle-income countries (LMICs).
Interpretation
RSV contributes substantially to morbidity and mortality burden globally in children aged 0–60 months, especially during the first 6 months of life and in LMICs. We highlight the striking overall mortality burden of RSV disease worldwide, with one in every 50 deaths in children aged 0–60 months and one in every 28 deaths in children aged 28 days to 6 months attributable to RSV. For every RSV-associated acute lower respiratory infection in-hospital death, we estimate approximately three more deaths attributable to RSV in the community. RSV passive immunisation programmes targeting protection during the first 6 months of life could have a substantial effect on reducing RSV disease burden, although more data are needed to understand the implications of the potential age-shifts in peak RSV burden to older age when these are implemented.
Related collections
Most cited references33


- Record: found
- Abstract: found
- Article: found