- Record: found
- Abstract: found
- Article: found
Evaluation and Endoscopic Management of Esophageal Submucosal Tumor
Read this article at
Abstract
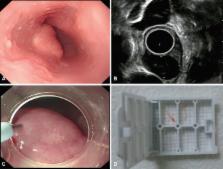
Submucosal tumors (SMTs) originate from tissues that constitute the submucosal layer and muscularis propria, and are covered by normal mucosa. Esophageal SMTs are rare, accounting for <1% of all esophageal tumors. However, the recent widespread use of endoscopy has led to a rapid increase in incidental detection of SMTs in Korea. Esophageal SMTs are benign in ≥90% of cases, but the possibility of malignancies such as gastrointestinal stromal tumor and malignant leiomyosarcoma still exists. Therefore, patients undergo resection in the presence of symptoms or the possibility of a malignant tumor. For resection of esophageal SMTs, surgical resection was the only option available in case of possible malignancy, but minimally invasive surgery by endoscopic resection is becoming more preferable to surgical resection with the development of endoscopic ultrasonography, endoscopic techniques, and other devices.
Related collections
Most cited references9
- Record: found
- Abstract: found
- Article: not found
Successful outcomes of a novel endoscopic treatment for GI tumors: endoscopic submucosal dissection with a mixture of high-molecular-weight hyaluronic acid, glycerin, and sugar.
- Record: found
- Abstract: found
- Article: not found
Esophageal leiomyoma: a 40-year experience.
- Record: found
- Abstract: not found
- Article: not found